Type 3 Endoleaks in Complex Endovascular Abdominal Aortic Aneurysm Repair within the Vascular Quality Initiative
Juliet Blakeslee-Carter, Adam W. Beck, Emily L. Spangler
University of Alabama at Birmingham, Birmingham, AL
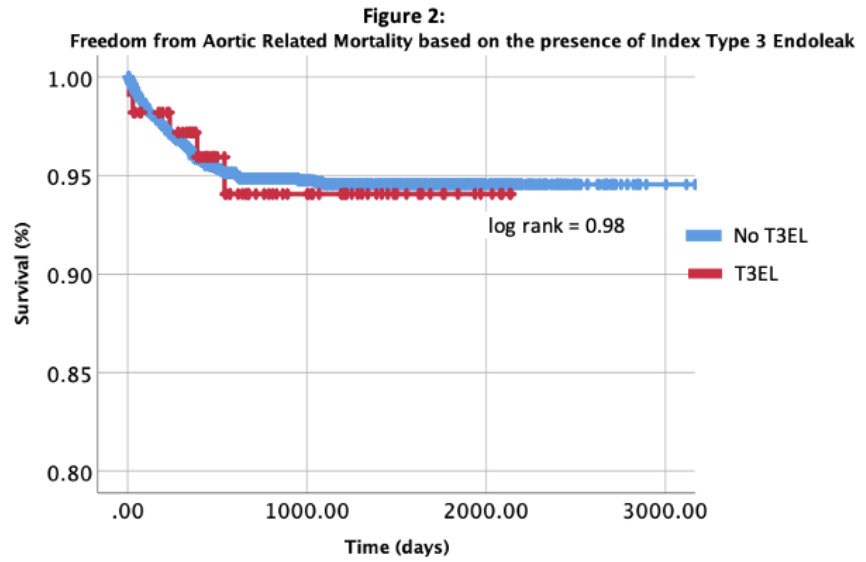
Background: The introduction of endovascular treatments revolutionized management of abdominal aortic aneurysms1,2. The dramatic evolution of endovascular technology now allows complex endovascular aortic aneurysm repair to address 25-30% of abdominal aneurysms with anatomy prohibitive to standard EVAR3. Utilization of complex EVAR, encompassing fenestrated/branched EVAR, physician modified endografts , and parallel stenting techniques (e.g. “chimney,” “snorkel,” and “sandwich” stents),4 has become increasingly common5,6. Despite engineering advances associated with complex EVAR, technical challenges and complications remain, including endoleaks. Type 3 Endoleaks (T3EL) occur due to modular device disconnection or graft fabric disruptions and are historically difficult to study due to their relative rarity. In prior database investigations of standard EVAR, the majority of T3EL are incident - not detected at the initial procedure but seen in follow-up, with incident T3EL associated with significantly increased mortality7. Evaluations of T3EL within complex EVAR have been limited to date. This study aims to evaluate the occurrence of T3EL in a national multicenter cohort, identify potential procedural characteristics associated with T3EL development, and determine their impact on clinical outcomes in complex EVAR. Methods: A retrospective review was conducted of all elective complex EVAR aortic aneurysm repairs within the Vascular Quality Initiative (VQI) between 2010 and March 2020. Complex EVAR was defined per VQI standards as thoracoabdominal repairs, suprarenal AAA, fenestrated/branched repairs, parallel stent repairs, custom manufactured devices, and physician modified endografts8, with the cohort limited to device deployment in Zone 5 or distal to exclude isolated TEVAR interventions. Standard definitions of endoleaks were used9. Endoleaks were evaluated within two key timeframes: index endoleaks occurring during index hospitalization, and incident endoleaks not present at index hospitalization, but occurring in long-term follow-up (defined as 9-21 months within the VQI). The primary end-point assessed was rate of Type 3 Endoleaks within complex EVAR, with secondary endpoints evaluating the impact of Type 3 Endoleaks on reintervention and survival. Results: A total of 4,070 complex EVAR cases were identified within the VQI database between 2010 and 2020. The average age was 73.3 ± 8.3 with an overall male predominance (74,1%).Half the cohort had a modified or custom graft (n=2055), with custom made grafts more common (80%) than physician modified devices (20%); the other half were presumed to have either snorkel or chimney repairs based on complex EVAR cohort definitions. The number of main body device components ranged from 1 (20.8%) to 6 (0.4%), with the majority having 2 main aortic body components implanted (n=2,493, 61.2%). The most common zone for device proximal deployment was Zone 8 (n=1,555, 38.2%). Type 3 Endoleaks at Index Hospitalization The overall index hospitalization T3EL rate was 4.1% (n=167). Figure 1 demonstrates cohort paths based on occurrence of T3EL, follow-up interventions, and mortality. The overall rate of any endoleak was 29.5% (n=1,203)(Table 1). The most common endoleaks were Type 2 (n=550, 13.5%), followed by Type 1 endoleaks (n=257, 6.3%). T3EL accounted for 14% of all index hospitalization endoleaks. A total of 33 T3EL (19.8%) occurred in conjunction with another endoleak; the most common endoleak to co-occur with a T3EL was a Type 2 Endoleak (n=17). On evaluation of pre-operative factors associated with development of index hospitalization T3EL, the only significant factors associated were custom/modified grafts (referent: unmodified device) and the number of device components. Devices with customization were more common in patients with T3EL (78.4% vs. 23.6%, p<0.001). Physician modified devices had significantly higher rates of T3EL compared to PMD (19.9% vs 10.2%, p<0.001). Devices with more than 1 component were significantly associated with index hospitalization T3EL (89.2% vs. 75.4%, p<0.001). Zone of proximal deployment had no significant association with the development of index T3EL. The overall rate of reintervention during index hospitalization was 6.0% (n=245), of which 195 (80%) were performed for aortic indications (database-defined as any treatment related to the aorta or branches involved with the index treatment) rather than access complications. Reinterventions for any endoleak type occurred in 0.6% (n=25/4,070), accounting for 13.1% of all aortic reinterventions (n=25/190) in complex EVAR during index hospitalization. Reinterventions for T3EL during index hospitalization were 0.36% (n=15/4,070), accounting for 60% of all endoleak reinterventions and 8.4% of all aortic reinterventions (n=16/190) (Figure 1). All T3EL that received reintervention at index hospitalization resolved and did not recur. Of the 16 patients that had reinterventions for T3EL during index hospitalization, 2 patients (12.5%) died following reintervention during that hospitalization. The presence of an index T3EL did not significantly affect the overall rate of reinterventions at index hospitalization (7.4% vs. 6%, p=0.52), but presence of an index T3EL was associated with reduced mean time to index hospitalization reintervention (1.4 ± 0.4 vs. 2.1 ± 0.6 days, p= 0.006). The overall mortality rate during index hospitalization was 3.9% (n=162). The all-cause mortality of T3EL at index hospitalization was 4.7% (n=8) versus 3.9% (n=154) in patients without index T3EL (p=0.59). Of the 8 patients with T3EL who died during index hospitalization, 2 (25%) received reintervention for T3EL and 4 (50%) had reintervention for other indications (1 access bleeding, 1 bowel ischemia, 1 type 1 endoleak, and 1 unspecified). When compared to patients without intervention for T3EL, patients with reintervention for T3EL during index hospitalization had a significantly higher index hospital mortality rate (13.3% vs. 3.9%, p=0.04). Type 3 Endoleaks at Follow-Up A total of 2,656 patients (68.0% taking in-hospital mortality into account), had follow-up data recorded. The overall rate of any incident endoleak at follow-up was 3.1% (n=82/2,656, Table 2), with Type 1 endoleaks the most common subtype (2.9%, n=76/2,656). Only one incident T3EL was seen at follow-up (0.04%), accounting for 1.2% of all incident endoleaks (n=1/82). Of the 13 patients with repaired T3EL that survived until discharge, 46.6% (n=7) had documented follow-up. Of the 146 unrepaired index T3EL that survived until discharge, 75% (n=109) had documented follow-up. Patients with an index T3EL made up 4.3% of the entire cohort (N=2,656) at follow-up (Figure 1). The overall rate of reintervention in complex EVAR at follow up was 7.9%, of which 195 (94%) were aortic reinterventions. Endoleak reinterventions occurred at a rate of 3.6% (n=97), which accounts for 50% of all aortic reinterventions done at follow-up. Reinterventions done for T3EL occurred at a rate of 0.7% (n=19), accounting for 20% of endoleak reinterventions (n=19/97) and 9.7% of all aorta-related reinterventions. The majority of T3EL requiring reintervention at follow-up were index T3EL unaddressed during index admission. Of the 19 patients with index T3EL that were repaired at follow-up, one patient presented with a rupture. The presence of an index T3EL or any T3EL was not significantly associated with reinterventions through 21 months of follow-up. Similarly there was no significant effect on time to reintervention. Cumulatively, at the end of the observational period, 12.8% of the cohort experienced mortality from any cause, and aortic mortality was 4.5% (n=120). On Kaplan Meier analysis, presence of an index hospital T3EL did not significantly decrease survival at 5 years (94% vs. 95%, log rank=0.904) (Figure 2). Reinterventions at LTF for T3EL did not significantly increase overall mortality or aortic mortality. Conclusion: Type 3 Endoleaks in complex EVAR are identified predominately at index placement rather than incident through 21-month follow-up. Index hospital reintervention for T3EL is significantly associated with increased perioperative mortality. While the presence of index T3EL did not significantly affect the rate of reintervention or 5-year mortality at follow-up, patients with these complications required earlier reinterventions and had shorter time until death. Unlike standard EVAR, where the presence of T3EL appears to influence long-term mortality, the clinical impact of a T3EL in complex repair may have different characteristics of onset due to differences in devices utilized, may be overshadowed by the incidence of type 1 endoleaks, or may result in more close monitoring due to early recognition during incident hospitalization. Factors that were significantly associated with the development of T3EL include higher device modularity and modified devices, suggesting that as devices continue to evolve, and undergo more complex modifications that the occurrence of T3EL may persist and require mindful management. Extending reporting intervals of endoleaks beyond the first year in registries would improve the ability to fully understand the impact of device fatigue and degeneration and more fully characterize the impact of T3EL.
Back to 2021 Abstracts