Back to 2017 Annual Meeting Program
Survival Following Fenestrated/Branched Endovascular Aortic Repair - Implications for Decision Making
Jocelyn M Beach, Jeevanantham Rajeswaran, F. Ezequiel Parodi, Yuki Kuramochi, Corey Brier, Eugene H Blackstone, Matthew J Eagleton
Cleveland Clinic, Cleveland, OH
BACKGROUND: Evolution of fenestrated/branched endovascular aneurysm repair (F/B-EVAR) is providing a less invasive approach to treating juxtarenal and thoracoabdominal aortic aneurysms (TAAA). Given its investigational nature, early applications of F/B-EVAR was predominantly directed towards patients considered high risk for conventional surgery. These procedures are performed with competitive perioperative morbidity and mortality; however, long-term outcomes are challenged by multiple, life-threatening co-morbidities. Enhanced understanding of factors contributing to the survival benefit of F/B-EVAR may allow for better patient selection and direct its application to those patients (both high- and standard-risk) who demonstrate a survival benefit. The aim of this study was to characterize mortality following F/B-EVAR and to identify risk factors associated with early peri-procedural and intermediate-term mortality.
METHODS: 1091 patients enrolled in a prospective F/B-EVAR, physician-sponsored, single-center IDE trial. The primary end point was all-cause mortality from the date of surgery. A non-proportional hazards multiphase model was built to model time-related mortality following surgery and its risk factors. These were further explored and verified by non-parametric random survival forest machine-learning technology.
RESULTS: Non-risk adjusted survival after F/B-EVAR was 97%, 85%, 64% and 46% at 30-days and 1, 3 and 5-years, substantially lower than that of the age-sex-race matched general population, but higher than high-risk untreated patients (Figure). Renal dysfunction (p=0.01), renal artery stenosis (p=0.01), thrombocytopenia (p<0.0001), and lower systolic blood pressure (p=0.005) were associated with higher early mortality. Higher heart rate (p=0.04), COPD (p=0.0001), congestive heart failure (p=0.006), lower ejection fraction (p=0.008), need for diuretics (p=0.01), anemia (p<0.0001), longer prothrombin time (p<0.0001), and larger aneurysms (0.0001) with a shorter infrarenal neck (p=0.0006) were risk factors for intermediate-term mortality. Type I/II extent TAAA repairs were associated with higher mortality both early and intermediate term.
CONCLUSIONS: Older patients with heart failure, COPD, renal dysfunction or occlusive disease, anemia, and coagulation disorders are at increased risk for death after F/BEVAR. This risk is highest in patients undergoing type I/II TAAA repairs and in those with larger aneurysms. Yet, even in this high-risk population with an often limited lifespan, F/B-EVAR is associated with greater survival than the natural history of untreated aortic aneurysms. Operative mortality in this high-risk population is lower than best open repair outcomes reported in the literature, suggesting a potential benefit in extending treatment of TAAA with F/B-EVAR to low and average risk patients.
Figure: Each circle symbol represents a death; vertical bars are confidence limits equivalent to ± 1 standard error, and solid lines enclosed within dashed 68% confidence bands equivalent to ± 1 standard error represent parametric estimates. Numbers in parentheses represent patients at risk beyond that point. For reference, the green dash-dot-dash line represents age-sex-race matched expected survival in the US population. Red dashed line represents survival for high-risk untreated AAA patients (referenced data). 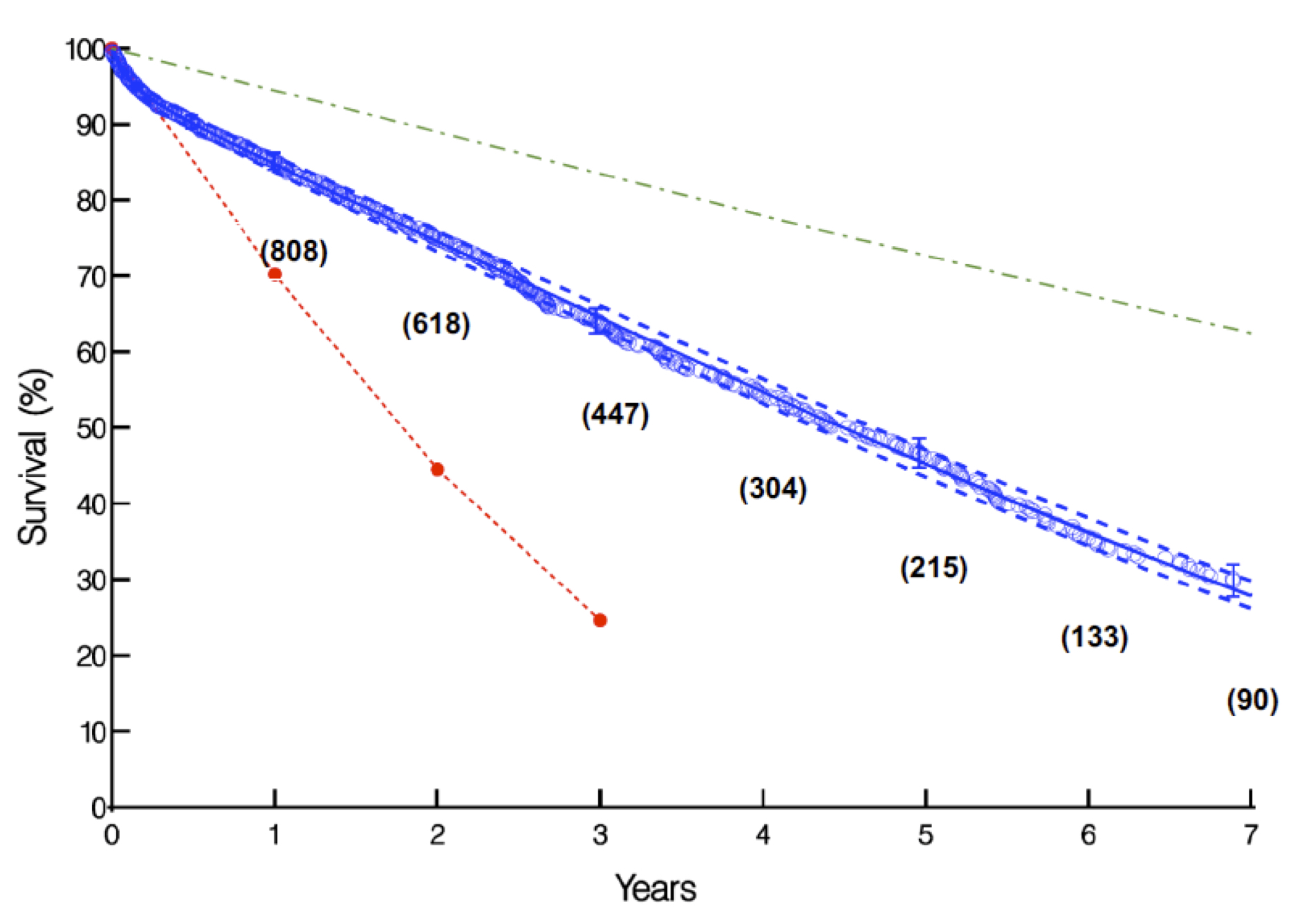
Back to 2017 Annual Meeting Program




