Back to 2017 Annual Meeting Program
Long-Term Results of Endovascular Repair for Descending Thoracic Aortic Aneurysms
David N Ranney, Morgan L Cox, Babatunde Yerokun, Ehsan Benrashid, Richard L McCann, G Chad Hughes
Duke University, Durham, NC
BACKGROUND - Since thoracic endovascular aortic repair (TEVAR) received US Food and Drug Administration (FDA) approval for the treatment of descending thoracic aneurysms in March 2005, excellent 30-day and midterm outcomes have been described. However, data on long-term outcomes is lacking with Medicare data suggesting that TEVAR has worse late survival compared to open descending repair. As such, the purpose of this study was to examine the long-term outcomes for on-label use of TEVAR for repair of descending thoracic aneurysm (DTA).
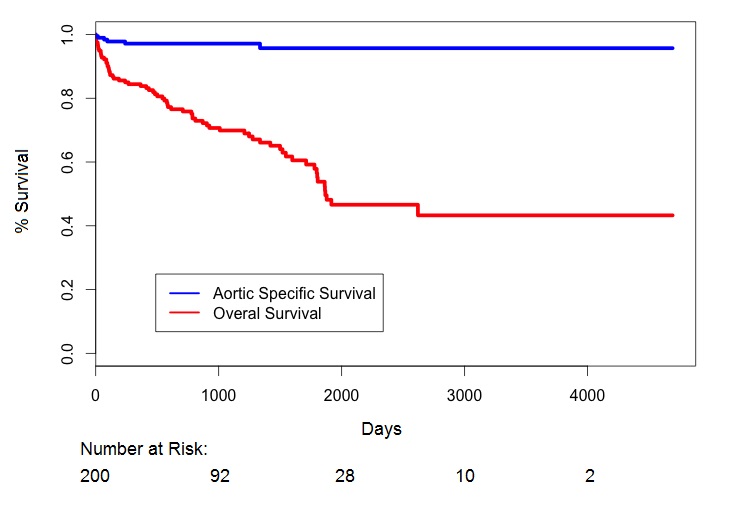
METHODS - Of 444 patients undergoing TEVAR between 3/2005 and 4/2016 at a single referral center for aortic surgery, 200 (45.0%) were performed for a descending thoracic aneurysm indication including 113 fusiform (56.5%), 81 saccular (40.5%), and 6 both saccular and fusiform (3.0%). All aneurysms were located distal to the left common carotid artery and proximal to the celiac axis, and hybrid procedures including arch or visceral debranching were excluded with the exception of left carotid-subclavian artery bypass. Aortic dissection and intramural hematoma as indications for TEVAR were also excluded. Primary 30-day/in-hospital outcomes included mortality, stroke, need for new permanent dialysis, and permanent paraparesis/paraplegia. Primary long-term outcomes included survival and rate of reintervention secondary to endoleak. The Kaplan Meier method was used to estimate long-term overall and aorta-specific survival.
RESULTS - Mean age was 71.0 ± 10.5 years (Table). All aneurysms were degenerative in nature with no patients with a connective tissue disorder. Mean aortic diameter was 5.8 ± 1.5 cm at time of intervention. Thirty-day rates of in-hospital mortality, stroke, permanent dialysis, and permanent paraparesis/paraplegia were 4.5%, 2.0%, 0.5%, and 1.0%, respectively. At a mean follow up of 35 ± 32 months (range 1-156), there were 61 late deaths (30.5%), 2 of which were due to aortic rupture. Actuarial overall and aorta-specific 13-year survival were 43.3% and 95.7%, respectively (Figure). Endovascular reintervention was required in 14 patients (6.9%) due to type I (N=10), type II (N=2), and type III (N=2) endoleak, all of which subsequently resolved. Zero patients required open reintervention for any cause.
CONCLUSIONS - Long-term (13-year) aorta-specific survival following endovascular repair of degenerative descending thoracic aneurysms in non-syndromic patients is excellent (96%) with a low rate of reintervention due to endoleak (7%), and endovascular repair should be considered the treatment of choice for this pathology. 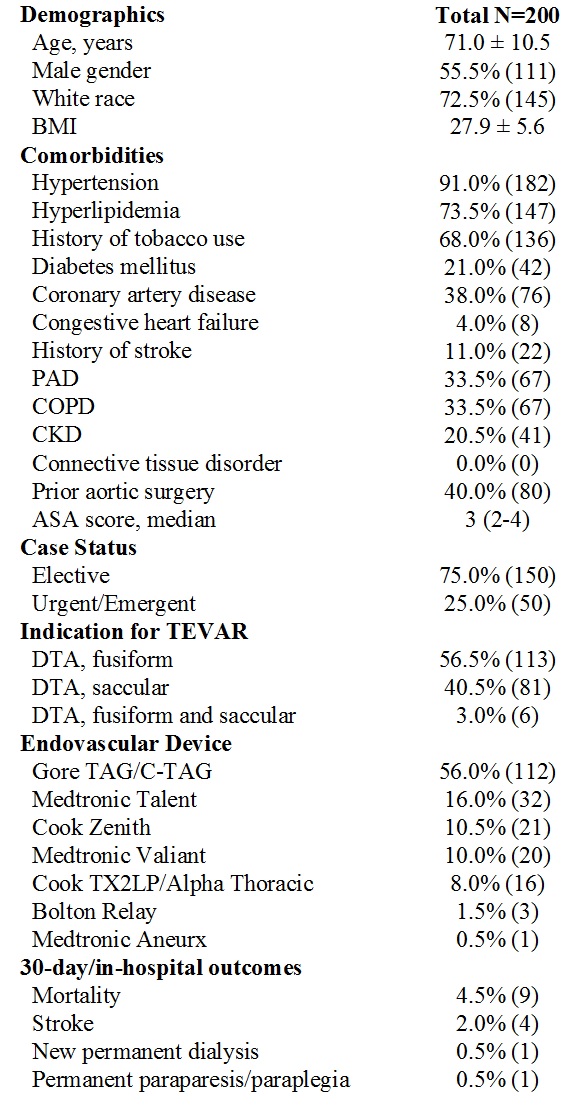
Back to 2017 Annual Meeting Program




