Back to 2017 Annual Meeting Program
High Hemoglobin A1c Associated With Increased Adverse Limb Events In Peripheral Arterial Disease Patients Undergoing Revascularization.
Shipra Arya1, Zachary O Binney2, Anjali Khakharia1, Luke P Brewster1, Peter W Wilson1, William D Jordan, Jr.1, Yazan Duwayri1
1Emory University, Atlanta, GA;2Rollins School of Public Health, Atlanta, GA
Introduction and Objectives: Diabetes mellitus (DM) and peripheral arterial disease (PAD) are independently associated with increased risk of amputation. However, the effect of poor glycemic control on adverse limb events has yet to be fully defined. In this study, we examined the effects of poor glycemic control as defined by high hemoglobin A1c (HbA1c>= 7.0%) on the risk of amputation and need for subsequent revascularization after lower extremity revascularization.
Methods: Patients undergoing PAD revascularization who had HbA1c levels available within 6 months before or after revascularization were identified in the VA database from 2003 to 2014 (N=26799). The diagnosis of preoperative DM (PreopDM) was defined using a primary clinic DM diagnosis code, 2 outpatient diagnosis codes or treatment for DM before the revascularization. Major amputation and MALE (amputation or need for subsequent revascularization) risk was measured at 30 days, 1 year and 5 years after revascularization. Cox proportional hazards models were created to assess the effect of high HbA1c on amputation/MALE (adjusted for covariates, including age, gender, race, SES, comorbidities, cholesterol levels, creatinine, supra/infrainguinal procedure, open/endovascular procedure and medications) for all patients and stratified on PreopDM.
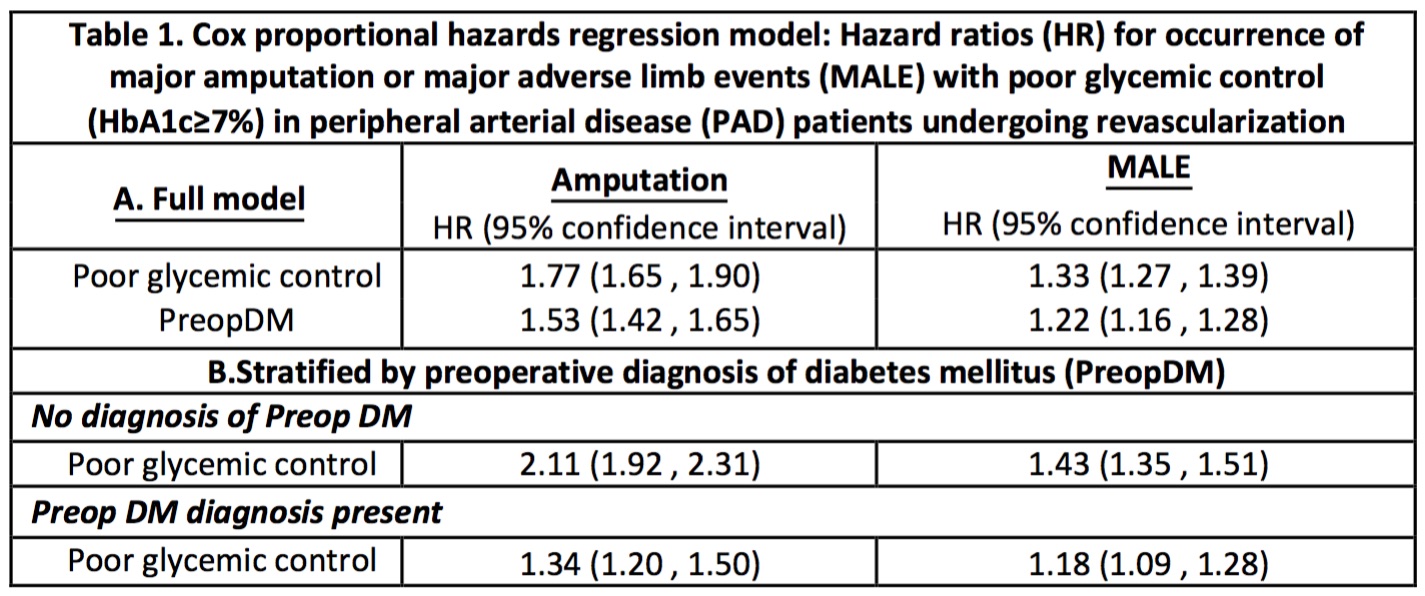
Results: High HbA1c levels were present in 33.2% of the cohort while 26.5% had PreopDM. Major amputations occurred in 4,359 (16.3%) patients and 10,580 (39.5%) had MALE in follow-up. Bivariate comparisons showed increased risk of amputation at 30 days, 1 and 5 years for patients with high HbA1c (5.8% vs 3.9%, 14.9% vs 9.0% and 21.1% vs 12.2% respectively; p<0.0001). MALE was also similarly higher in patients with high HbA1c at each time point (11.4% vs 8.8%, 32.6% vs 25.6% and 44.4% vs 34.8% respectively; p<0.0001). Kaplan Meier curves showed worst outcomes in patient with PreopDM and high HbA1c (Figure 1). In the Cox model, High HbA1c was associated with a 77% higher amputation risk and 33% higher MALE risk as compared to patients with normal glycemic control while a preoperative diagnosis of DM was associated with a 53% and 22% increase in amputation and MALE risk as shown in Table 1. In stratified analysis the relative risk of amputation/ MALE was much higher with poor glycemic control in patients without a pre-operative diagnosis of diabetes as compared to those with it [Table 1].
Conclusion: PAD patients with poor perioperative glycemic control (HbA1c>=7.0%) have a significantly higher risk of amputation and MALE than patients with good glycemic control. Poor glycemic control in patients without a preoperative diagnosis of DM carries twice the relative risk of amputation and MALE than those with good glycemic control. These results suggest that screening of diabetic status and management of glycemic control could be a target for improvement of perioperative and long term outcomes in PAD patients. 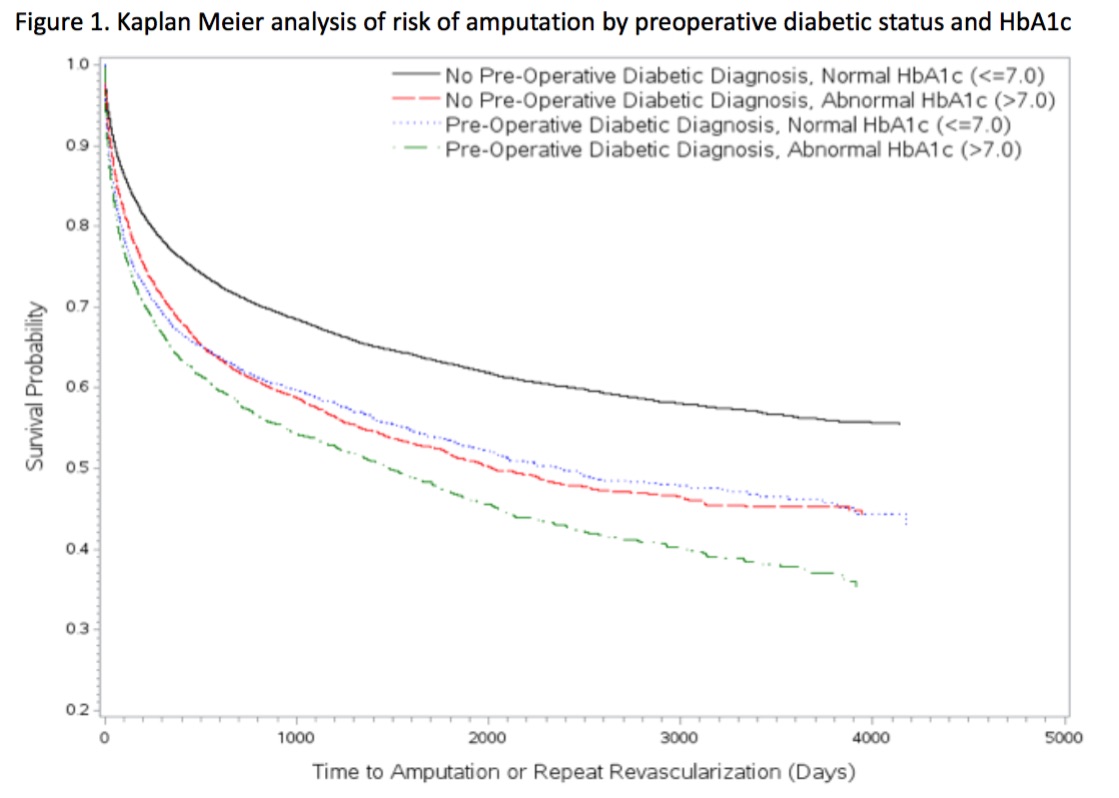
Back to 2017 Annual Meeting Program




