Back to 2017 Annual Meeting Program
Improving Outcomes and Value with Staged Hybrid Extent II Thoracoabdominal Aortic Aneurysm Repair
Robert B Hawkins1, J. Hunter Mehaffey1, Adishesh K Narahari1, Amit Jain2, Ravi Ghanta1, Irving L Kron1, John A Kern1, Gilbert R Upchurch1
1University of Virginia, Charlottesville, VA;2University of Cincinnati, Cincinnati, OH
Background: Complex Crawford extent II thoracoabdominal aortic aneurysms (TAAA) can be treated in a hybrid manner with proximal thoracic endovascular aneurysm repair (TEVAR), followed by staged distal open thoracoabdominal repair. The purpose of this study was to evaluate the outcomes and healthcare associated value of this new method compared to traditional open repair over 10 years.
Methods: A prospectively collected database was used to identify all patients with extent II TAAA undergoing repair at a single institution between 2005 and 2015. Patient characteristics, post-operative outcomes, and incidence of major adverse events (MAE = renal failure, spinal cord ischemia, death) were compared. Value was analyzed looking at quality (1/MAE) divided by inflation adjusted total health system cost.
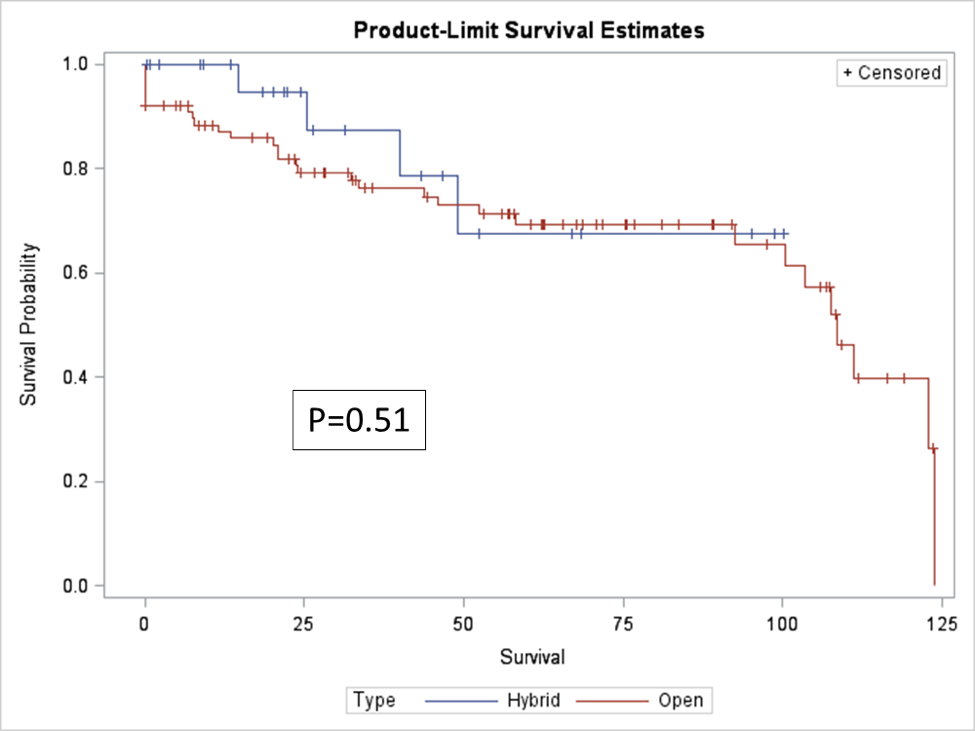
Results: 113 consecutive patients underwent extent II TAAA repairs, of which 25 (22.1%) had a staged hybrid approach with a median of 129 days between procedures. No baseline differences in demographic or comorbidity variables existed between groups (p>0.05). The hybrid group had shorter operative time (255 vs 306 minutes, p=0.01), shorter postoperative length of stay (LOS) (10.1 vs 13.3 days, p=0.02), and reduced blood loss (1,300 vs 2,600 mL, p=0.01) at the time of open operation. Despite higher rates of acute kidney injury in the hybrid group (76.0% vs 51.1%, p=0.03) there was no difference in renal failure (8.0% vs 4.5%, p=0.84). The incidence of MAE was significantly lower in the staged hybrid group (20.0% vs 48.9%, p=0.01), while in-hospital mortality (4.0% vs 3.4%, p=0.89) and long-term survival were not different (Kaplan Meier p=0.51; Figure 1). Median total cost was higher in the hybrid group ($112,920 vs $72,037; p=0.01). The hybrid approach resulted in over 50% increased value (156 vs 100; Table 1).
Conclusions: Staged hybrid repair of complex extent II TAAA results in lower LOS, blood loss, operative time and MAE. The increased costs of hybrid repair are offset by improved outcomes resulting in improved value over open repair.
Table 1. Healthcare Associated Value
| Variable | Staged Hybrid | Standard Open | p-value |
| Major Adverse Event | 5 (20.0%) | 43 (48.9%) | 0.017 |
| Total Cost (median) | $112,920 | $72,037 | 0.003 |
| Value | 156 | 100 |
Total cost was adjusted for inflation and represents 2015 dollars.
Figure 1. Kaplan Meier Survival Plot (months)
Back to 2017 Annual Meeting Program




