Back to 2017 Annual Meeting Program
Impact of Early versus Late Timing of TEVAR On Aortic Remodeling and Long-Term Survival Following Type B Aortic Dissection
Babatunde A Yerokun, Muath Bishawi, Adam R Williams, David N Ranney, Ehsan Benrashid, Richard L McCann, G. Chad Hughes
Duke University Medical Center, Durham, NC
INTRODUCTION:Lack of false lumen thrombosis (FLT) after thoracic endovascular aortic repair (TEVAR) for Type B aortic dissection is a significant predictor of mortality during follow-up. Limited literature examines the role that timing (early versus late) of TEVAR after Type B aortic dissection impacts FLT and long-term survival. This study examined the association of timing of TEVAR after Type B aortic dissection on FLT and survival during long-term follow-up.
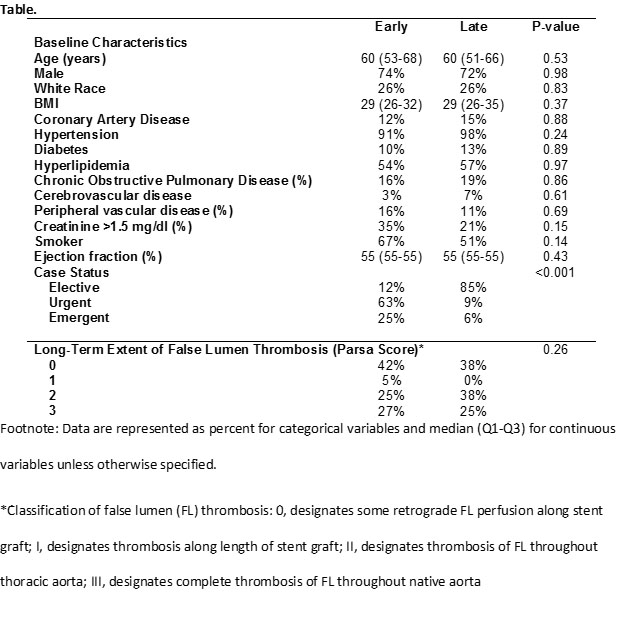
METHODS:N=110 consecutive patients who underwent TEVAR for Type B aortic dissection between July 2005-April 2016 were identified from a prospectively maintained institutional aortic surgery database. Hybrid procedures or those requiring aortic debranching were excluded. Of the 105 patients with follow-up imaging, 55 patients underwent TEVAR ≤3 months (early; mean interval to TEVAR 0.7 months [IQR 0.1-0.3]) after Type B aortic dissection and 48 patients underwent TEVAR >3 months (late; mean interval to TEVAR 6.3 months [IQR 4.0-7.0]) after Type B aortic dissection. The primary endpoint was the degree of FLT in the descending aorta. The extent of FLT was graded using the Parsa Score (Table legend). Follow-up imaging was independently reviewed by two blinded reviewers before a consensus decision was made. Secondary endpoints included long-term overall and aorta-specific survival. Chi-square and t-tests were used for outcome comparison. Survival analyses were calculated using the Kaplan-Meyer method.
RESULTS:Baseline patient characteristics were similar between the early and late TEVAR groups (Table). Extent of FLT was not different between the two groups on latest postoperative imaging surveillance with a mean follow-up of 39.1 months in the early group and 33.6 months in the late group (Table). The mean length of covered aorta was significantly shorter in patients undergoing early TEVAR (20.7cm vs. 23.5cm, p=0.03). Additionally, the early TEVAR group received significantly fewer endografts (1.6 vs. 2.0, p=0.01). Overall long-term survival was significantly higher in those undergoing early compared to late TEVAR (KM 7-yr: 93.8% vs. 70.8% respectively; p=0.044), although there was no difference late aorta-specific survival between the early and late groups (KM 7-yr: 100.0% vs. 95.3% respectively; p=0.121) (Figure).
CONCLUSIONS:In patients with Type B aortic dissection, the timing of TEVAR (early vs late) was not associated with the degree of FLT and aortic remodeling during follow-up, although patients who underwent TEVAR within 3 months of their dissection event required significantly shorter aortic pavement and fewer devices to achieve this similar degree of aortic remodeling. Similarly, long-term aorta-specific survival was not different for patients undergoing TEVAR for Type B dissection whether treated early or late. These data suggest that delaying TEVAR after dissection until aortic complications develop may not compromise the ability to prevent aorta-related death, although additional study, ideally with randomized controlled trials, is needed. 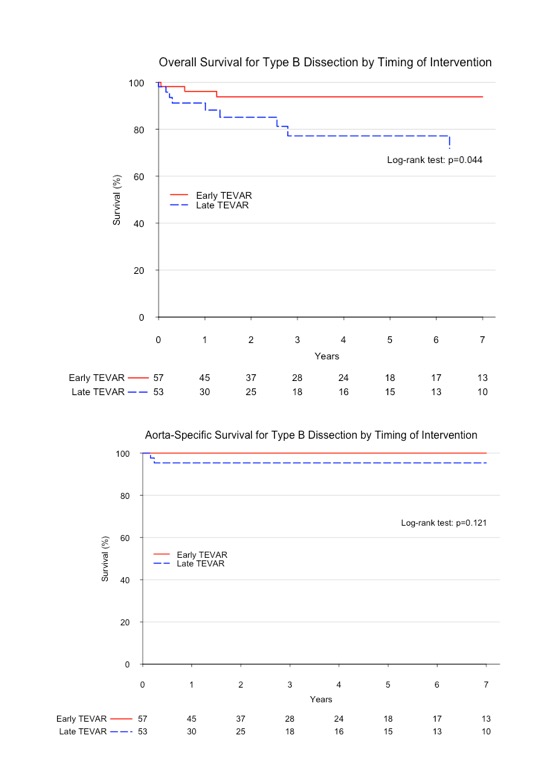
Back to 2017 Annual Meeting Program




