Back to 2017 Annual Meeting Program
Importance of Post-Procedural Wound, Ischemia and Foot Infection (WIfI) Restaging in Predicting Limb Salvage
Charles Leithead, Emily Spangler, Marc Passman, Zdenek Novak, Adam Witcher, Mark Patterson, Adam Beck, Benjamin Pearce
University of Alabama at Birmingham, Birmingham, AL
INTRODUCTION:
The Wound, Ischemia, foot Infection (WIfI) classification system was created to encompass demographic changes and expanding techniques of revascularization in order to perform meaningful analysis of outcomes in the treatment of critical limb ischemia (CLI). WIfI index is intended to be analogous to the TNM staging system for cancer, with restaging to be done after control of infection and after revascularization. We previously demonstrated that preoperative wound and infection grades are predictive of limb loss, while ischemia grade is not. Our goal was to evaluate the effectiveness of WIfI restaging after therapy in the prediction of limb loss.
METHODS:
Preoperative WIfI scoring was performed prospectively on all CLI patients who underwent revascularization from January 2014 to June 2015. WIfI restaging and assessment of outcomes was performed retrospectively using our vascular database and electronic medical records through August 2016. WIfI classification was determined preoperatively, immediately postoperative, and at one and six months after intervention. Amputation-free survival was the primary endpoint. Kaplan-Meier plot analysis and comparisons of preoperative grades to respective postoperative grades were performed utilizing paired t-test, Chi-square and correlation analyses.
RESULTS:
A total of 180 CLI patients underwent revascularization, of which 29 had major amputations (16%). Wound grades generally improved following surgery across the entire cohort. Major amputation was associated with preoperative wound grade and remained associated with wound grade at postoperative restaging at 1 month and beyond based on amputation frequency analysis (preoperative, one, and six months p=0.03, <0.001, <0.001, respectively). Wound grade was significantly associated with amputation-free survival at one and six months after intervention (LogRank <0.001 for restaging intervals). Ischemia grades improved initially with a slight decline across the cohort at six months: patients with ischemia grade 0 or 1 (ABI ≥ 0.6) were 20.6% of the cohort preoperatively, improving to 70.7%, 85.8% and 77.6% immediately postoperative, one and six months, respectively. Ischemia grade at one month postoperative was associated with amputation free survival (Figure 1), LogRank 0.03. Foot infection grades also improved at each time interval. The proportion of patients with no signs of infection (grade 0) were 74.4%, 85.4%, 87.0% and 95.8% preoperatively, immediately postoperative, one and six months postoperative, respectively. Foot infection grade at one month postoperative was associated with amputation-free survival (Figure 1), LogRank <0.001, as well as at six months (LogRank 0.017).
CONCLUSIONS:
WIfI restaging is an important tool for predicting limb loss and assessing adequacy of intervention, more so than baseline WIfI alone. One month postoperative ischemia grade correlated with amputation free survival while preoperative grade did not. One month postoperative wound and foot infection grades additionally correlated with amputation free survival. WIfI restaging at one month postoperative may help identify a cohort which remains at higher risk for limb loss and may merit reintervention. 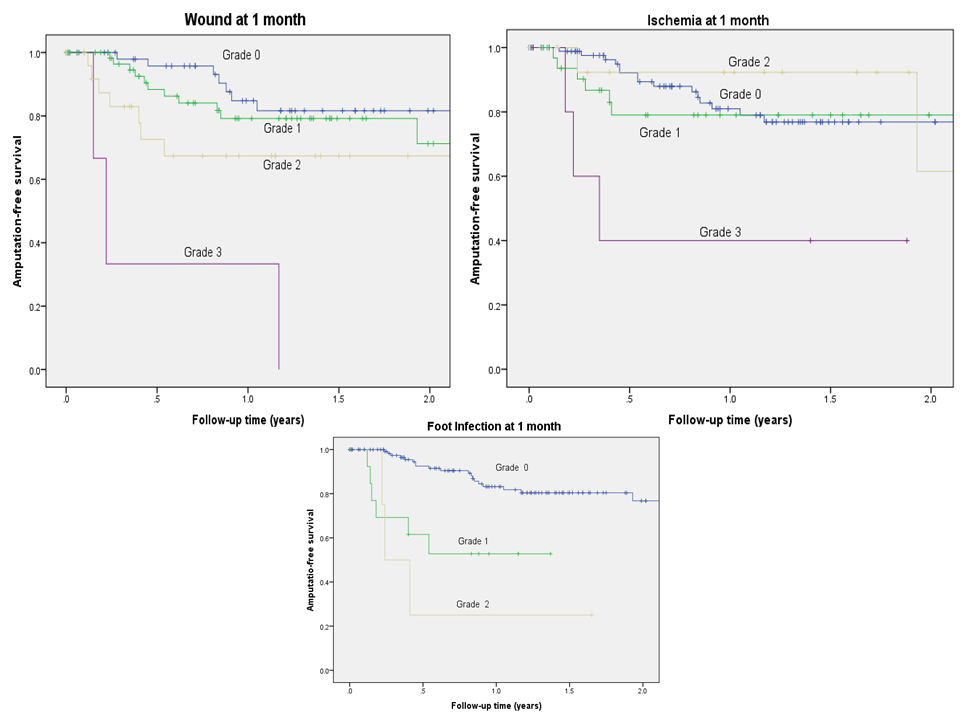
Back to 2017 Annual Meeting Program




