Back to 2017 Annual Meeting Program
Isolated Lower Extremity Vasculitis Leading to Progressive Critical Limb Ischemia
Pouria Parsa, Anthony Rios, Lisa N Anderson, John F Eidt, Bradley Grimsley
Baylor University, Dallas, TX
BACKGROUND
According to autopsy studies and improving vascular imaging techniques, large vessel involvement of the extremities may be more prevalent than we once thought. The prevalence of lower extremity GCA findings according to the largest series of histologically documented extracranial GCA is 18%. While limb claudication may be present in conjunction with systemic signs of inflammation, classic cranial manifestations, or preexisting diagnosis of PMR on initial diagnosis of GCA, even more rare are patients presenting with isolated lower extremity claudication or ischemia preceding their GCA diagnosis.
Because limb-restricted GCA is rarely described, there is no consensus on medical and surgical management. Steroid therapy is well known to treat constitutional symptoms associated with GCA, however, reports vary on whether or not they prevent progression and aid in resolution of occlusive lesions or whether these lesions remain refractory to therapy. In our review, patients have been shown to develop ischemic complications after initiation of steroid therapy. Immunosuppressive drugs either as an alternative or given in conjunction with steroids have been studied but have unknown efficacy with inconclusive evidence supporting their use in the literature.
CASE REPORT
Our patient is a 67-year-old woman with significant cardiac history who was seen in the emergency department with 3 week history of bilateral lower extremity rest pain. Her workup was significant for bilateral lower extremity occlusive disease with elevated ESR. She was started on steroids and monitored closely until her inflammatory markers improved. Following resolution of her inflammatory state, she underwent bilateral lower extremity revascularization. An intraoperative biopsy of the SFA was sent for permanent pathology which was consistent with GCA. The biopsy was analyzed in two cross sections as shown in Figure 1.0. One cross section contained a partial to near completely occluded lumen with evidence of chronic inflammation, fibrin, and fibrosis. The mural chronic inflammatory cell infiltrate was comprised of lymphocytes and mononuclear cells with scattered rare multinucleated giant cells. The microscopic findings were consistent with vasculitis and suggested a diagnosis of giant cell arteritis.
Patient had an uncomplicated post-operative course. She was seen in Vascular Surgery clinic one month following her discharge, she denies claudication or rest pain like symptoms.
CONCLUSIONS
Increased awareness of the different manifestations of GCA is crucial for diagnosis of patients with isolated lower extremity vasculitis. It is imperative that GCA be considered in the differential diagnosis of unexplained lower extremity claudication especially in patients with few risk factors for atherosclerotic disease, rapidly progressive disease, elevated inflammatory markers, and characteristic findings on imaging. With advances in imaging identifying a higher prevalence of limb involvement than previously thought, consideration must be given to systemic screening methods to assess for limb vasculitis with the potential for rapid progression to critical limb ischemia. Further studies with systemic imaging and longer follow-up are necessary to clarify optimal imaging studies and treatment methods in limb-restricted GCA. 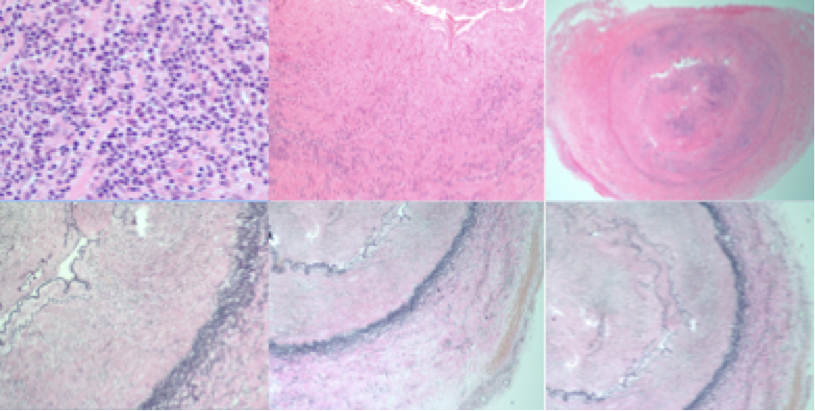
Back to 2017 Annual Meeting Program




