Back to 2017 Annual Meeting Program
Bridging the Gap: Intra-operative Cone-beam CT Guided Endovascular Recanalization of an Interrupted Aortic Arch
Philip L Auyang
Houston Methodist Hospital, Houston, TX
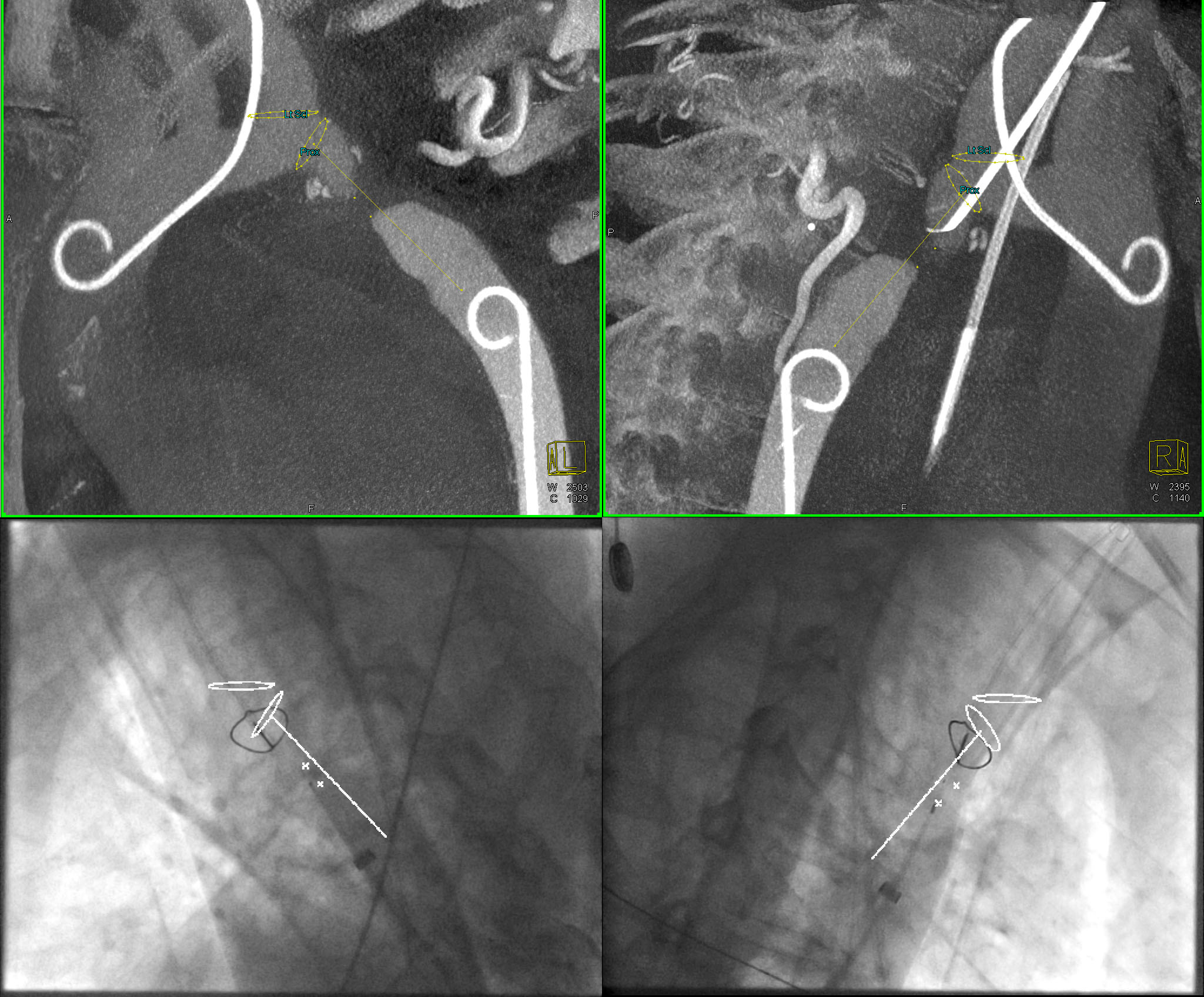
INTRODUCTION: This case presentation describes a novel percutaneous image-guided endovascular repair of a completely interrupted aorta utilizing radiofrequency perforation wire to highlight the value of pre-operative planning and intra-operative rotational cone-beam CT (CBCT) (syngo DynaCT, Siemens Medical Solutions USA Inc.). Here we propose that enhancing 2D fluoroscopy with 3D landmarks obtained from intra operative CBCT rendered a complex case to be performed with relative finesse.
METHODS: A 42-year old man presented after sustaining an MCA territory stroke secondary to malignant hypertension. In clinic he was found to have a 70 mmHg differential peak-to-peak gradient between upper and lower extremity. Pre-operative CT demonstrated complete interruption of the aorta distal to the origin of the left subclavian artery with extensive collateral circulation (Figure 1). In the hybrid suite 2D fluoroscopy was enhanced with 3D landmarks corresponding to proximal and distal points of the interruption, centerline trajectory of the aorta, and the left subclavian ostium (Figure 2). These were used to direct a 0.024” Nykanen radiofrequency guidewire (Baylis Medical, Montreal, Canada) within a coaxial catheter to approach the interruption in a retrograde fashion, from femoral artery access, avoiding critical adjacent structures most notably the left pulmonary artery. The electronic markers derived from CBCT were tracked in real-time with changes in C-arm angulations, table positions, and image zoom. Successful perforations were achieved with a single attempt and the wire was snared proximally from radial artery access. An arterio-arterial loop was created and the distal sheath was advanced carefully through the interrupted segment and snugly into the proximal sheath. This system was then advanced antegrade into the distal pouch and docked within a 14 french sheath and again advanced retrograde to dilate the tract with minimal bleeding. At this point a 18mm x 4.5cm balloon expandable covered Cheatham-platinum stent (NuMED Inc., Hopkinton, NY) was successfully deployed to bridge the interruption.
RESULTS: Immediately after the procedure the gradient decreased significantly and the patient was discharged post-operative day one with an uneventful hospital course. Clinical follow up 10 months after the procedure revealed that the patient’s hypertension had been normalized on only low doses of beta blocker and calcium channel blocker therapy.
CONCLUSIONS: This case presentation demonstrates that appropriate and better utilization of integrated, multi-modality 3D information in the operating suite can be one of the major factors determining better clinical outcomes. Additionally, we found this technique to have the potential to reduce overall fluoroscopy time and nephrotoxic dye administration compared to standard biplane angiography when undertaking complex vascular anatomical cases. In summary, such novel intra-operative 3D imaging, image fusion and guidance tools facilitate better integration of 3D pre-operative planning to the actual procedure and holds great promise to approach complex interventions in a safe and efficacious manner.

Back to 2017 Annual Meeting Program




