Back to 2017 Annual Meeting Posters
Improved Outcomes with Proximal Radiocephalic Arteriovenous Fistulas Compared to Brachiocephalic Arteriovenous Fistulas
Dean J Arnaoutakis, Elise P. Deroo, Patrick McGlynn, Maxwell D. Coll, Dirk M Hentschel, Michael Belkin, C. Keith Ozaki
Brigham and Women's Hospital, Boston, MA
Background:
Brachiocephalic arteriovenous fistulas (BCF) are associated with high-flow volumes leading to potential risks such as arm swelling, steal syndrome, pseudoaneurysm (due to a pressurized access), and cephalic arch stenosis. We hypothesized that a proximal radiocephalic fistula (prRCF) configuration mitigates these risks since a lower-flow state is created. Furthermore, we also hypothesized that despite these lower flows, patencies (primary, primary-assisted, secondary) are sustained.
Methods:
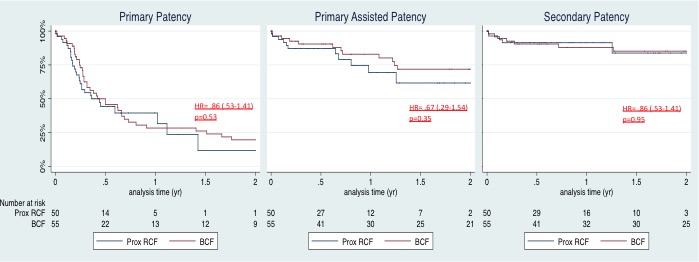
Leveraging a prospectively collected database supplemented with detailed medical record data, analyses of patients undergoing BCF and prRCF were completed (November 2008 through March 2016). Preoperative clinical and imaging characteristics, operative variables, and postoperative complications were reviewed. The primary endpoint was a composite of arm swelling, steal, and pseudoaneurysm at 2 years. Fistulagrams and interventions (surgical revision, thrombectomy, endovascular treatment of cephalic arch stenosis) censored at 2 years were compared between configurations. Patencies were plotted using Kaplan Meier techniques and compared using Cox-proportional hazards.
Results:
During the study period 345 arteriovenous fistulas and 72 prosthetic grafts were primarily placed. 56 patients underwent BCF and 50 prRCF with a mean follow up of 1.8±1.7(SD) years. Besides RCF patients being older, there was no difference between the groups with regards to preoperative characteristics. The artery diameter used for anastomosis was significantly larger in the BCF group (4.0±1.1mm vs 2.6±0.8mm, p<.001) with higher flow volumes at 6-week ultrasound (1,060±587mL/min vs 735±344mL/min, p<.001). Complications (arm swelling, steal, pseudoaneurysm) were significantly more common in the BCF group (p=.003). There was a trend for the BCF group to require more cephalic arch stenosis interventions (Table 1). Of those patients needing dialysis within 1 year, both BCF and prRCF were successfully used in the majority of patients (n=27, 66% vs n=25, 63%, p=1.0). Unadjusted and adjusted primary, primary-assisted, and secondary patency rates were similar between the groups (Figure 1).
Conclusions:
prRCF have fewer complications yet similar durability compared to BCF. When anatomically feasible, prRCF should be constructed over BCF due to their superior physiology and clinical outcomes.
Table 1. Outcomes within Two Years
| Variables | BCF (n=56) | RCF (n=50) | P-value |
| Mean 6-week flow volume, ml/min (SD) | 1060 (587) | 734 (344) | .003 |
| Patients with complications, # (%) | 14 (25) | 2 (4) | .003 |
| Arm swelling, # (%) | 5 (9) | 1 (2) | |
| Pseudoaneurysm, # (%) | 8 (14) | 0 (0) | |
| Steal syndrome, # (%) | 5 (9) | 1 (2) | |
| Fistulagram, # (%) | 36 (64) | 29 (58) | .55 |
| Interventions | |||
| Surgical revision | 7 (18) | 7 (14) | .75 |
| Patch venoplasty, # (%) | 2 (4) | 1 (2) | |
| New anastomosis, # (%) | 1 (2) | 1 (2) | |
| Interposition/jump graft, # (%) | 2 (4) | 4 (8) | |
| Banding, # (%) | 2 (4) | 2 (4) | |
| Pts with cephalic arch intervention, # (%) | 13 (23) | 6 (12) | .13 |
| Side branch ligation, # (%) | 22 (39) | 22 (44) | .70 |
| Superficialization, # (%) | 17 (30) | 11 (22) | .38 |
Figure 1. Primary, Primary-Assisted, and Secondary Patency Rates
Back to 2017 Annual Meeting Posters




