Comparative Outcomes of Open, Hybrid, and Fenestrated Branched Endovascular Repair of Extent II and III Thoracoabdominal Aortic Aneurysms
Dean J. Arnaoutakis, Salvatore T. Scali, Adam W. Beck, Thomas S. Huber, Andrew J. Martin, Liza F. Laquian, Thomas M. Beaver, Gilbert R. Upchurch
University of Florida- Gainesville, Gainesville, FL
INTRODUCTION: Open repair of Crawford extent II and III thoracoabdominal aortic aneurysms(TAAA) is associated with substantial perioperative risk. In an effort to reduce this risk, endovascular technologies are increasingly utilized and include either a hybrid operation combining proximal thoracic endovascular aortic repair and staged open distal TAAA repair(Hybrid) or a total endovascular approach using fenestrated/branched endografts(FEVAR). However, the benefits of these alternative approaches compared to open surgery remains unclear. The purpose of this study was to compare outcomes of these three different strategies in the management of Extent II/III TAAA.
METHODS: All patients undergoing extent II/III TAAA repair(2002-2018) for non-mycotic, degenerative aneurysm or chronic dissection related indications by the division of vascular surgery at a single institution were identified. The primary end-point was 30-day mortality. Secondary end-points included incidence of spinal cord ischemia(SCI), complications, unplanned reoperation and/or 90-day readmission, and survival. To mitigate impact of covariate imbalance and selection bias, inter-group comparisons were made using inverse-probability weighted(IPW) propensity analysis. Cox regression was used to estimate survival while cumulative incidence was employed to determine re-operation risk.
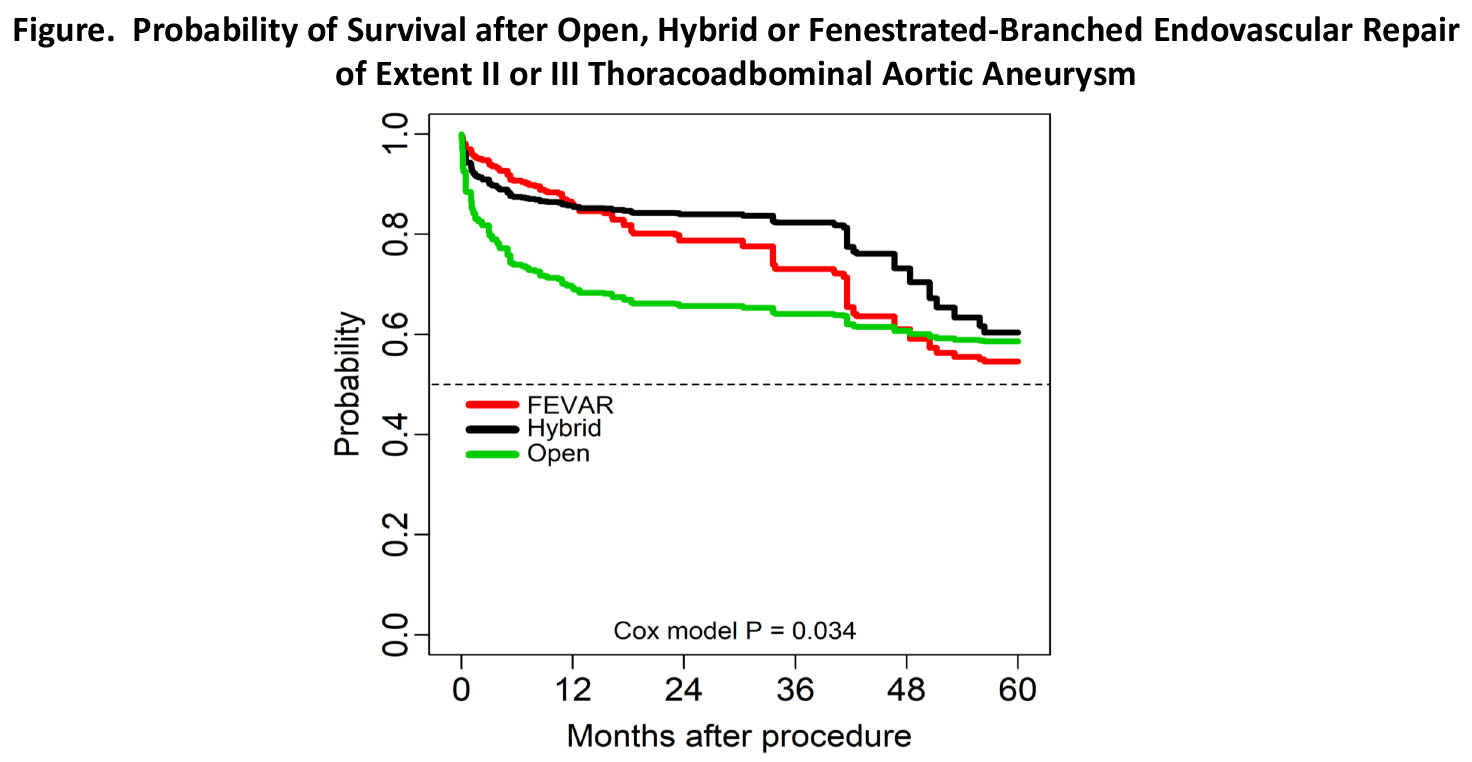
RESULTS: 198 patients(FEVAR=92, Hybrid=40, Open=66) underwent extent II/III TAAA repair. Seven(18%) Hybrid patients were excluded in adjusted analysis because they never underwent the 2nd stage operation(death=5;lost follow-up=2). In unadjusted analysis, compared to Hybrid/Open patients, FEVAR subjects were significantly older with more cardiovascular risk factors, but less likely to have a connective tissue disorder or a dissection-related indication. The unadjusted 30-day mortality and complication risks were: 30-day mortality, FEVAR-4%, Hybrid-13%, Open-12%(p=0.01);complications, FEVAR-36%, Hybrid-33%, Open-50%(p=0.11)[Permanent SCI: FEVAR-3%, Hybrid-3%, Open-6%(p=0.64)%]. In adjusted analysis, 30-day mortality risk was significantly greater for Open vs. FEVAR[HR 3.6, 95%CI 1.4-9.2, p=.008] with no difference for Hybrid vs. Open or Hybrid vs. FEVAR(Table). There was significantly lower risk of any SCI for FEVAR patients compared to Open(Open:FEVAR, 3.4, 1.0-11.3;p=.04); however, there was no difference overall in the risk of permanent SCI. There was no difference in risk of major complications or unplanned reoperation but Hybrid patients had greater risk of unplanned 90-day readmission compared to FEVAR/Open subjects(Table). There was a time varying effect of procedure type on survival probability between 30 and 90 days with Open repair having greater mortality risk. This led to a significant 1-year but not 5-year survival disadvantage of Open vs. Hybrid/FEVAR subjects(1 and 5-year survival: FEVAR, 86±3%, 55±8%; Hybrid, 86±5%, 60±11%; Open 69±7%, 59±8%;Cox-model p=0.03;Figure).
CONCLUSIONS: Extent II/III TAAA repair, regardless of operative strategy, is associated with significant morbidity risk. FEVAR is associated with the lowest 30-day mortality risk compared to Hybrid and Open repair when patients are matched based upon preoperative risk factors. These data support greater adoption of FEVAR as first-line therapy to treat complex TAAA disease in anatomically suitable patients who present electively. 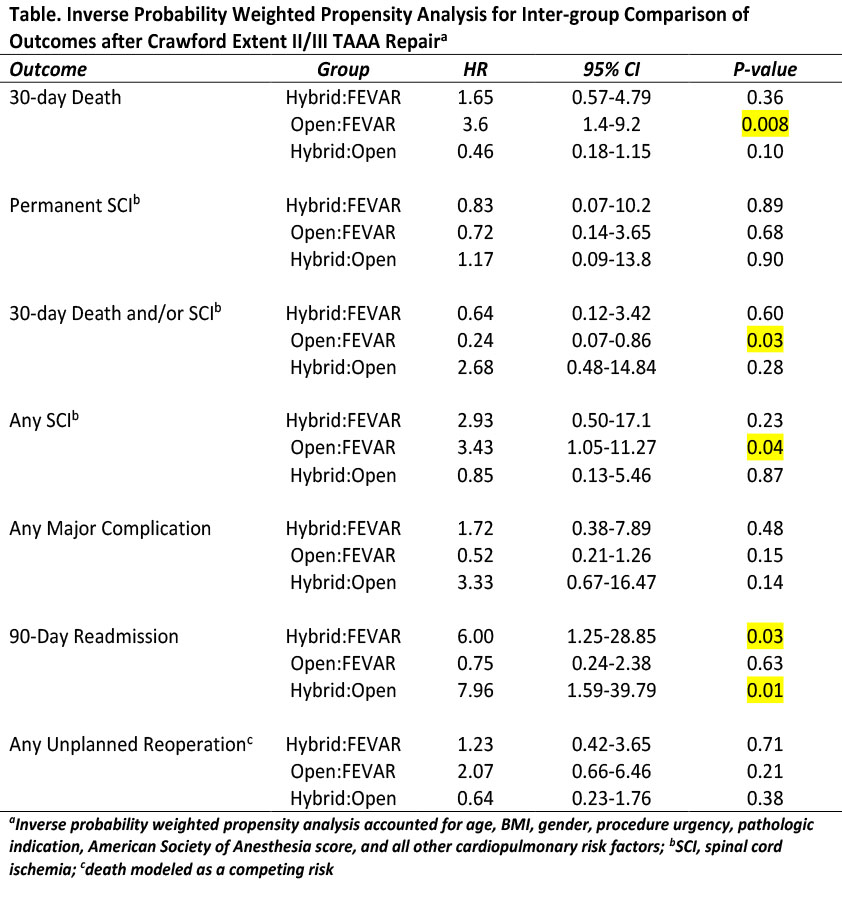
Back to 2019 Abstracts
