Clinical Outcome of Drug-Eluting Balloon Angioplasty in Patients With Femoropopliteal Disease: Real World Single Center Experience
Ali F AbuRahma, Zachary AbuRahma, Grant Scott, Elliot Adams, Matthew Beasley, Meghan Davis, L. Scott Dean, Elaine Davis
Robert C. Byrd Health Sciences Center of W. Va. Univ., Charleston, WV
INTRODUCTION: Several multicenter industry sponsored clinical trials reported satisfactory results in the use of drug-eluting balloons (DEB) for treatment of femoropopliteal occlusive disease. However, few single center studies were published to verify the outcome from real world experience.
METHODS: This is a retrospective analysis of 228 patients (mean age 68 years) treated with DEB angioplasty (Lutonix 0.35, Bard) during 7 year period. 30-day perioperative MAEs (major adverse events) (death, amputation, target lesion thrombosis/reintervention) were calculated. Kaplan-Meier Analysis was used to estimate primary and assisted primary (APP) patency rates (based on duplex ultrasound ± ABI), freedom from reintervention, and limb salvage rates.
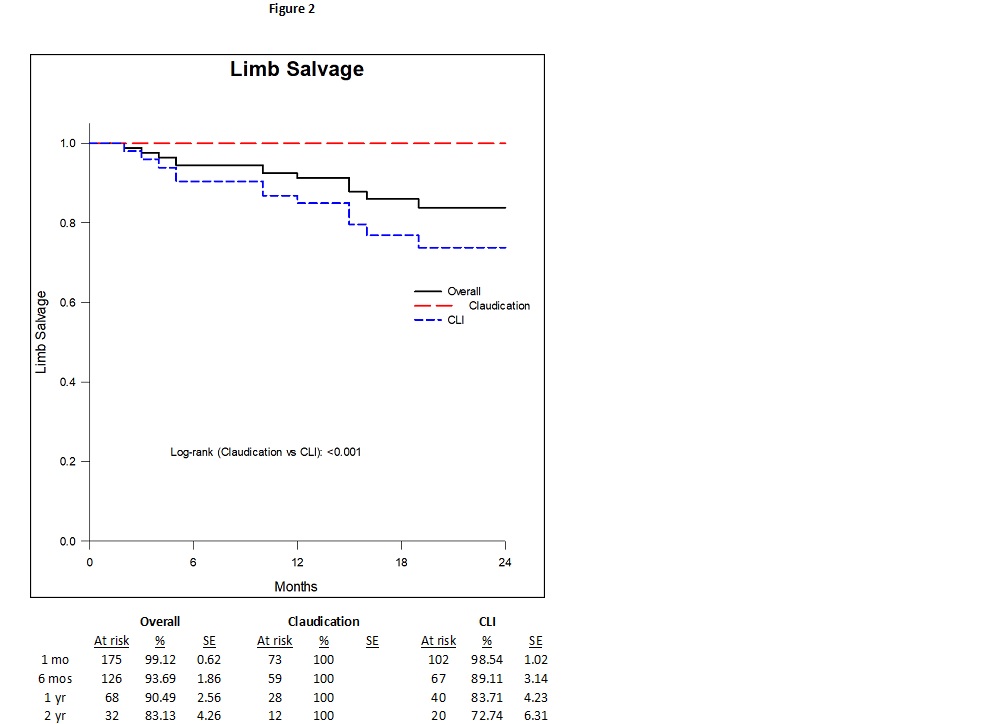
RESULTS: Lesions treated were primarily TASC C&D. Indications included Rutherford category 2&3 (claudications) in 40% and critical limb ischemia (CLI) (R-4&5) in 60%. Lesions treated: 61% SFA, 15% popliteal artery (PA), and 24% in both SFA and PA. Mean follow-up was 12 months (range 1-89). Overall 30-day perioperative morbidity and mortality rates were 13% and 1%. 30-day perioperative MAE rate was 3%. Symptom relief (improvement of ≥ one Rutherford category) was obtained in 64%. Primary patency rates were 55% and 35% and APP rates were 67% and 46% at 1 and 2 years, respectively. Rates of freedom from reintervention were 76% and 56% at 1 and 2 years. Limb salvage rates were 90% and 83% at 1 and 2 years.
When patients were classified according to indications of intervention, there were more femoral arteries treated in patients with claudications (70% vs 54% for CLI, P=.0382). Patients with claudications had a lower rate of early perioperative complications (4% vs 19%, P=.0014). Symptom improvement was 77% for claudication vs 56% for CLI (P=.0014). Overall, major amputation rate was 0% for claudication vs 13% for CLI (P=.0003).
The primary patency rates at 1 and 2 years were 58% and 38% for claudication vs 53% and 33% for CLI (P=.2) (Figure 1). The APP rates at 1 and 2 years were 70% and 47% for claudication vs 64% and 44% for CLI (P=.307). The rates of freedom from reintervention at 1 and 2 years were 81% and 66% for
claudication vs 72% and 49% for CLI (P=.09). Limb salvage rates at 1 and 2 years were 100% and 100% for claudication vs 84% and 73% for CLI (P<.001) (Figure 2).
CONCLUSIONS: Clinical outcomes after DCB angioplasty in femoropopliteal lesions were inferior to what has been reported in previous studies. Further investigation from real world experience with long-term follow-up is needed to confirm these results. 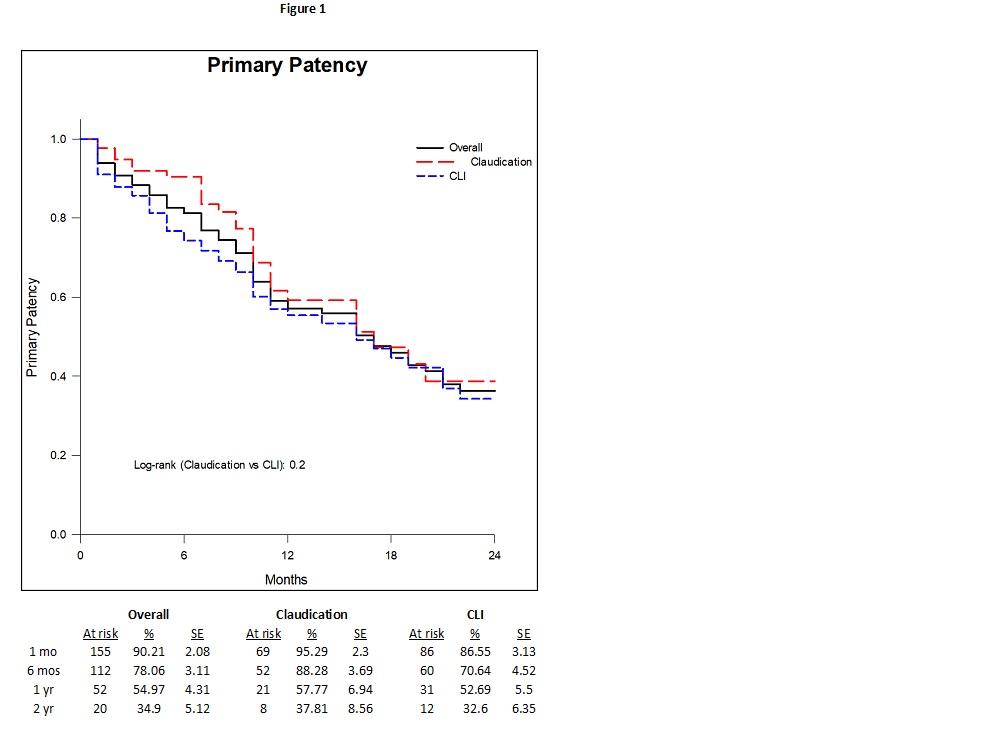
Back to 2019 Abstracts
