Influence of Gender and Frailty on Mortality after Elective Aortic Aneurysm Repair
Sarah Barbey1, Lusine Yaghjyan1, Paul Kubilis1, Adam W. Beck2, Philip Goodney3, Kristina A. Giles1, Thomas S. Huber1, Gilbert R. Upchurch1, Salvatore T. Scali1
1University of Florida- Gainesville, Gainesville, FL;2University of Alabama-Birmingham, Birmingham, AL;3Dartmouth-Hitchcock Medical Center, Lebanon, NH
INTRODUCTION: Controversy exists surrounding gender outcome disparity and abdominal aortic aneurysm(AAA) repair. Previous reports have demonstrated worse outcomes for female patients undergoing open aortic repair(OAR); however, these differences are less evident with endovascular repair(EVAR). Epidemiological studies have documented that non-surgical, female patients score higher on most frailty assessment scales but paradoxically have longer life-expectancy compared to male subjects. Notably, the interaction of gender/frailty and their influence on outcomes and practice patterns surrounding EVAR/OAR is poorly described. The purpose of this analysis was to characterize gender/frailty effects on patient selection and mortality after elective AAA repair in the Society for Vascular Surgery Vascular Quality Initiative(SVS-VQI).
METHODS: All elective infrarenal AAA(EVAR+OAR;2003-2017) cases were queried from the VQI database. Each patient was assigned a previously published modified Frailty Index(mFI) score derived from comorbidity and preoperative functional status data. The mFI was analyzed as a discrete continuous variable(0-9) and categorized into three strata(0-2, 3-5 and 6-9). The cohorts were further stratified by gender and procedure type and analyzed using multivariable Cox proportional hazard models, adjusted for statistically-significant covariates including procedure complexity(p<0.05).
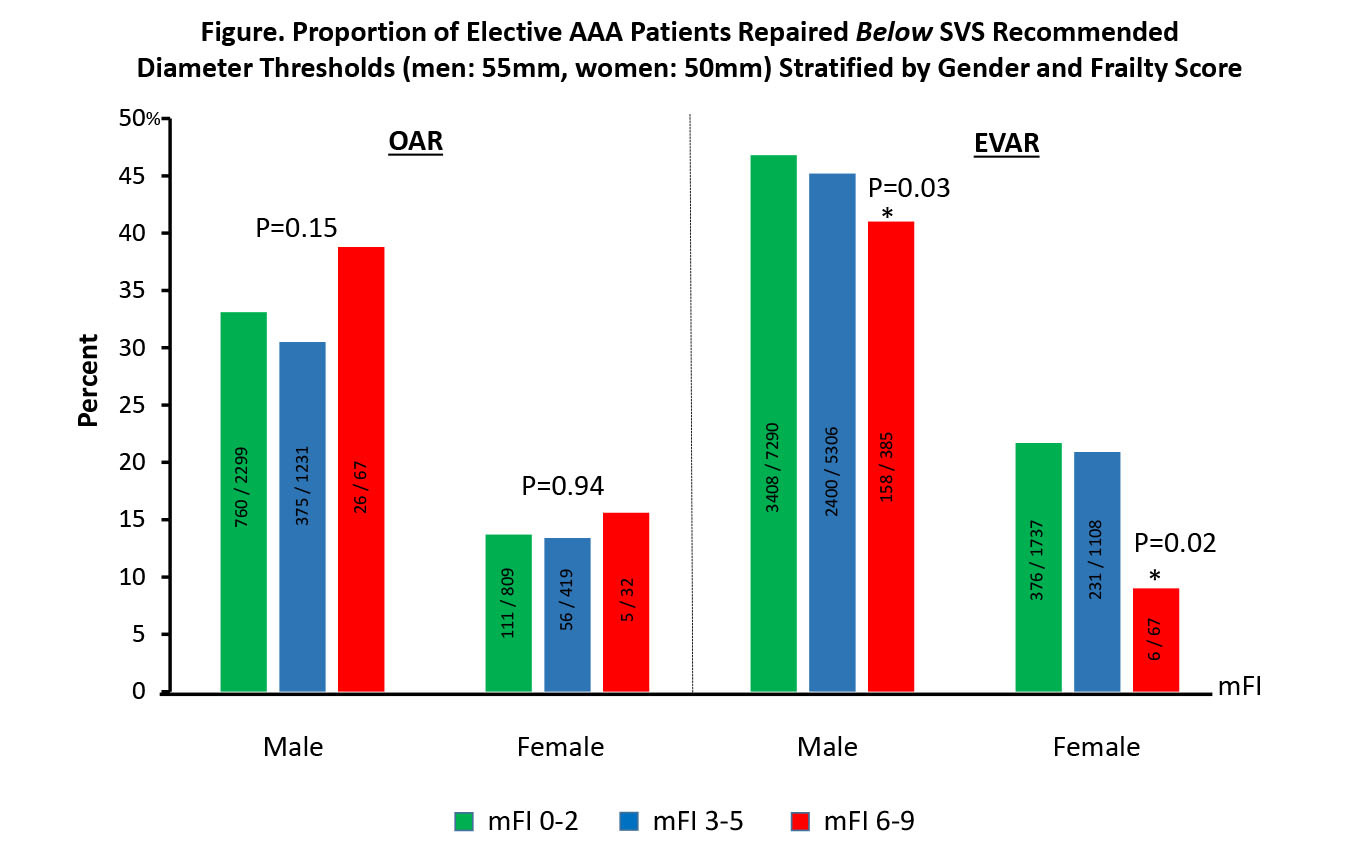
RESULTS: A total of 20,750 elective AAA cases were analyzed[EVAR-15,893(77%);OAR-4857(23%)]. 30-day mortality for EVAR and OAR was 0.7%(N=115) and 3.5%(N=169), respectively. Patients who died were significantly more likely to be older(EVAR-78 vs. 73;OAR-74 vs. 69yrs;p<0.0001), have larger AAA diameters(EVAR-59 vs. 56mm;p=0.005;OAR-62 vs. 59mm;p=0.001), higher mFI scores(EVAR-3.2 vs. 2.4;OAR-3.1 vs. 2.2;p<0.0001), and be female gender(EVAR-29% vs. 18%;HR 1.66[95% CI 1.10-2.52];p=0.007;OAR-36% vs. 26%;1.43[1.02-1.99];p=0.003). Significant differences in the gender distribution of frailty scores among EVAR patients was evident(mean mFI:male-2.42 vs. female-2.34;p=0.02) but no difference was detected for OAR(male-2.17 vs. female-2.22;p=0.38). mFI was a strong independent predictor of mortality(30-day: EVAR-HR 1.36[1.22-1.53], OAR-1.46[1.32-1.60];1-year: EVAR-1.32[1.25-1.39], OAR-1.38[1.28-1.48]). For any specific mFI score, female patients were more likely to experience 30-day mortality(Table). Across frailty strata, male patients were nearly 2-fold more likely to undergo either elective EVAR or OAR for an AAA below recommended minimum diameter thresholds(male<5.5cm;female<5.0cm). Greater mFI score did not alter OAR selection but was associated with less frequent EVAR of small AAA(Figure).
CONCLUSIONS: Female patients are significantly more likely to die compared to male subjects after both elective endovascular and OAR infrarenal AAA repair. Female patients have similar or lower mFI scores relative to male patients; however, when matched by mFI score and controlling for procedural complexity, female subjects are more likely to experience postoperative death. This indicates that the mFI does not account for unmeasured factors contributing to worse outcomes among women and requires further study to delineate the cause of this outcome disparity. There are significant gender differences in patient selection based upon current SVS endorsed treatment guidelines which has important implications on the appropriateness of AAA care delivery nationally. 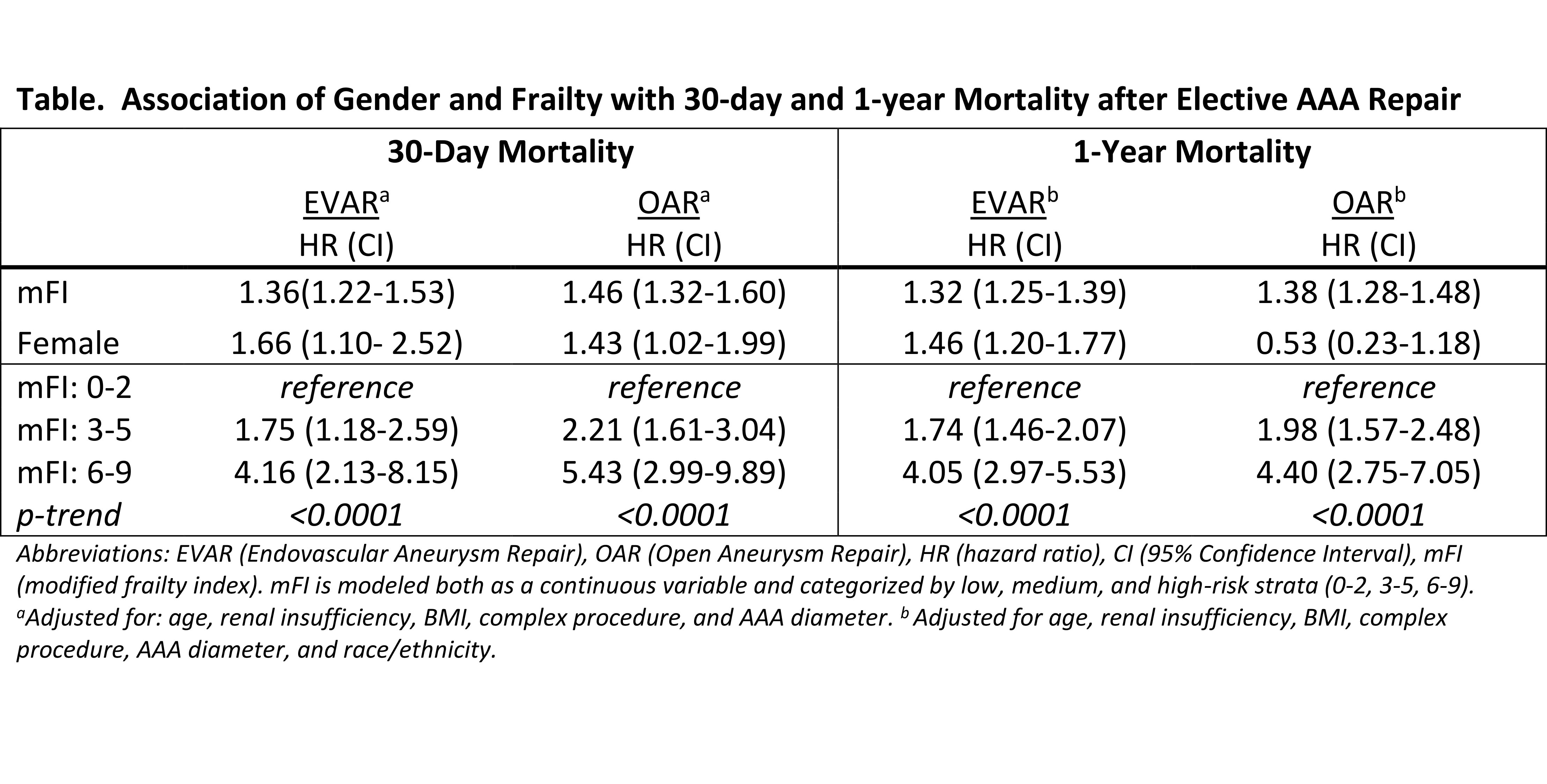
Back to 2019 Abstracts
