Effects of Statin and Antiplatelet Therapy Noncompliance and Intolerance on Patient Outcomes following Vascular Surgery
Johnston L Moore, Zdenek Novak, Graeme E McFarland, Mark A Patterson, Marc A Passman, Emily L Spangler, Benjamin J Pearce, Adam W Beck
University of Alabama at Birmingham School of Medicine, Division of Vascular Surgery and Endovascular Therapy, Birmingham, AL
Effects of Statin and Antiplatelet Therapy Noncompliance and Intolerance on Patient Outcomes following Vascular Surgery
Moore JL, Novak Z, McFarland GE, Patterson MA, Passman MA, Spangler EL, Pearce BJ, Beck AW
University of Alabama at Birmingham School of Medicine, Division of Vascular Surgery and Endovascular Therapy. Birmingham, AL
Background:
Prior studies have evaluated the effects of statin and antiplatelet (AP) medications on the vascular surgery patient population. While the benefits of statin and AP usage are well described, there is a paucity of research into the specific outcomes of patients who are unable to take the medication due to intolerance or noncompliance. Our goal is to examine the outcomes of intolerant patients and to compare to those who are noncompliant.
Methods:
We performed a retrospective study of patients within the Vascular Quality Initiative (VQI) registry undergoing an elective procedure between 2005-2018. Patients who died within 30 days postoperatively and those missing data were removed. Patients were considered noncompliant if they were previously prescribed a medication at discharge but were not taking it at 1-year follow-up or if patient-reported "noncompliant" in the VQI. Medication intolerance was defined if listed as "no, for medical reasons" in the VQI. Mortality data was ascertained using the Social Security Death Index (SSDI).
Results:
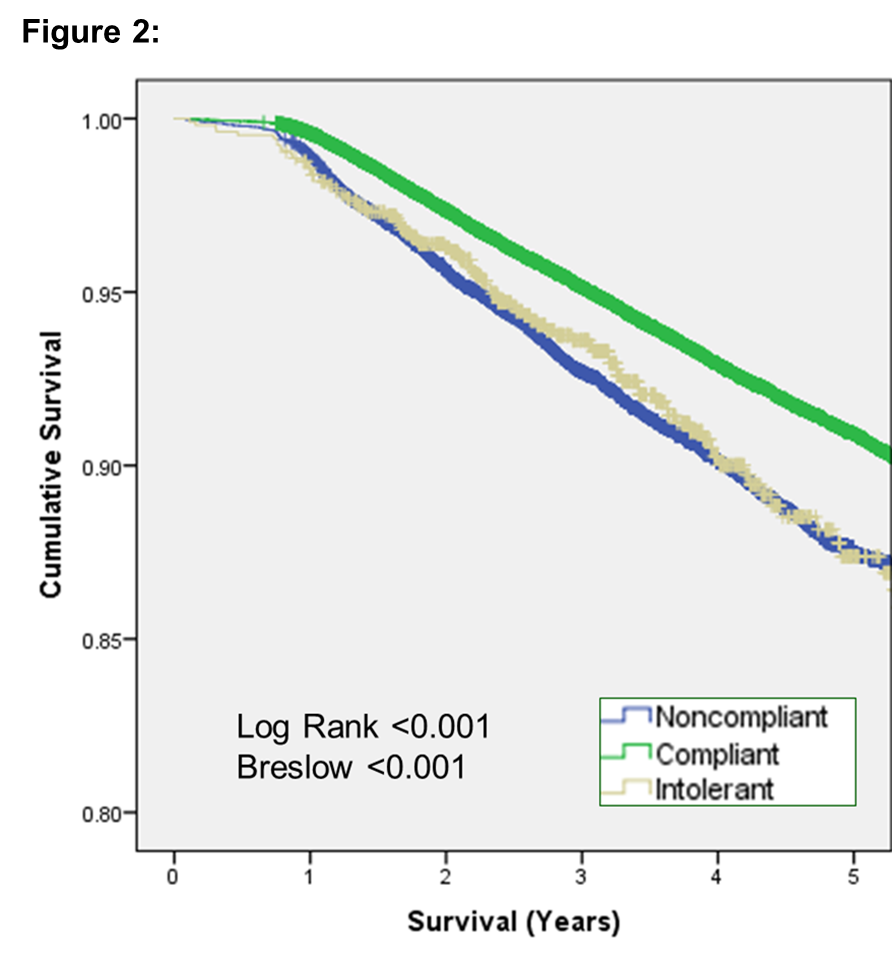
We identified 140,010 patients that met our inclusion criteria. Statin intolerance was noted in 2.3% at discharge and 2.1% at 1-year follow-up, with 0.7% listed as intolerant at all stages. Statistically significant factors associated with increased risk of medication intolerance included female gender, lower extremity procedures, insurance (non-U.S. insurer), discharge destination (nursing home), and documented intolerance to other medications (ACE-I, ASA, anticoagulants, and beta-blockers). Survival analysis (Figure 1) revealed 91% survival at 5 years in patients on both statins and AP agents compared to 82% in patients taking neither medication (Log Rank <0.001). As seen in Figure 2, patients with statin intolerance have a similar survival course to noncompliant patients. Noncompliance at 1 year for statins, aspirin, and P2Y12 inhibitors was 9.0%, 11.8%, and 28.9% respectively. Noncompliance with statins was correlated with noncompliance to aspirin (R=0.16, p<0.001) and to P2Y12 inhibitors (R=0.09, p<0.001). Statistically significant factors associated with increased risk of medication noncompliance included female gender, lower extremity procedures, insurance (self-pay), discharge destination (nursing home), and ambulatory status (requiring assistance).
Conclusions:
Patients not taking statin and AP therapy have a substantially decreased 5-year survival irrespective of the reason for not taking. Although noncompliance can be quite difficult to manage, intolerant patients may be more engaged and benefit from alteration of statin dose or type (hydrophilic vs. lipophilic), or the use of newer agents, such as PCSK9 inhibitors. 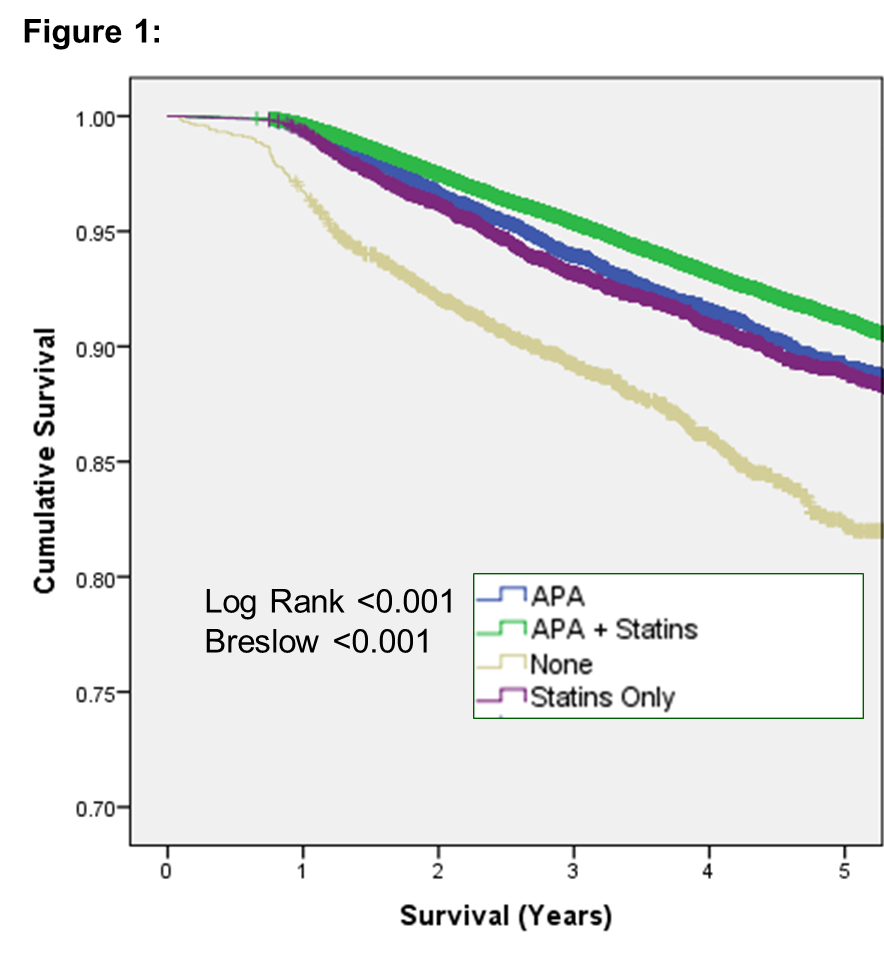
Back to 2019 Abstracts
