Influence of Hospital Volume on Patient Selection, Risk of Complications, and Mortality from Failure to Rescue after Open Abdominal Aortic Aneurysm Repair
Kristina A. Giles1, Thomas S. Huber1, Gilbert R. Upchurch1, Adam W. Beck2, Dean Arnaoutakis1, Martin R. Back1, Salvatore T. Scali1
1University of Florida- Gainesville, Gainesville, FL;2University of Alabama at Birmingham, Birmingham, AL
INTRODUCTION: The effect of hospital volume (HV) on mortality after open abdominal aortic aneurysm repair (OAAA) is well known; however, the underlying mechanism for improved outcomes is poorly understood. Better patient selection, lower risk of complications, and improved ability to rescue patients after adverse events are assumed mechanisms, but little data exist to validate this hypothesis. The purpose of this analysis was to determine the influence of HV on patient selection, incidence of complications and failure to rescue (FTR) after adverse events resulting from OAAA repair.
METHODS: The Vizient database (>95% of all academic hospitals) was reviewed for OAAA repairs (elective, n=2827; non-elective, n=1622) performed from 2013-2015. Presentation type (elective vs. non-elective) was considered in all analyses. Elixhauser comorbidity index (EI) and Walraven-weighted scores (EWS) were assigned to patients and volume-outcome relationships explored. Using logistic regression, risk-adjusted complication (including preventable complications; Agency for Healthcare Research and Quality patient safety indicators-PSIs) and FTR rates were determined. Predicted risk scores were assigned to delineate HV effects on these outcomes.
RESULTS: Overall, no relationship between HV and composite patient comorbidity score was identified (EI and EWS: Pearson= [Rho .02], P=0.2; [Rho -0.01], P=0.4); Spearman correlation coefficient = [Rho 0.02], P=0.4; [Rho-0.02], P=0.2). The lack of correlation persisted when considering elective vs. non-elective status. However, for elective cases, differences in specific comorbidities were noted since HV hospitals were more likely to repair patients with a history of peripheral vascular disease (P=0.01), diabetes (P=0.07), obesity (P=0.004), and alcohol abuse (P=0.05). Lower volume hospitals more frequently repaired patients with hypothyroidism (P=0.05), fluid and electrolyte disorders (P=0.007), and chronic blood loss anemia (P=0.05). No specific individual comorbidity differences were detected for non-elective cases.
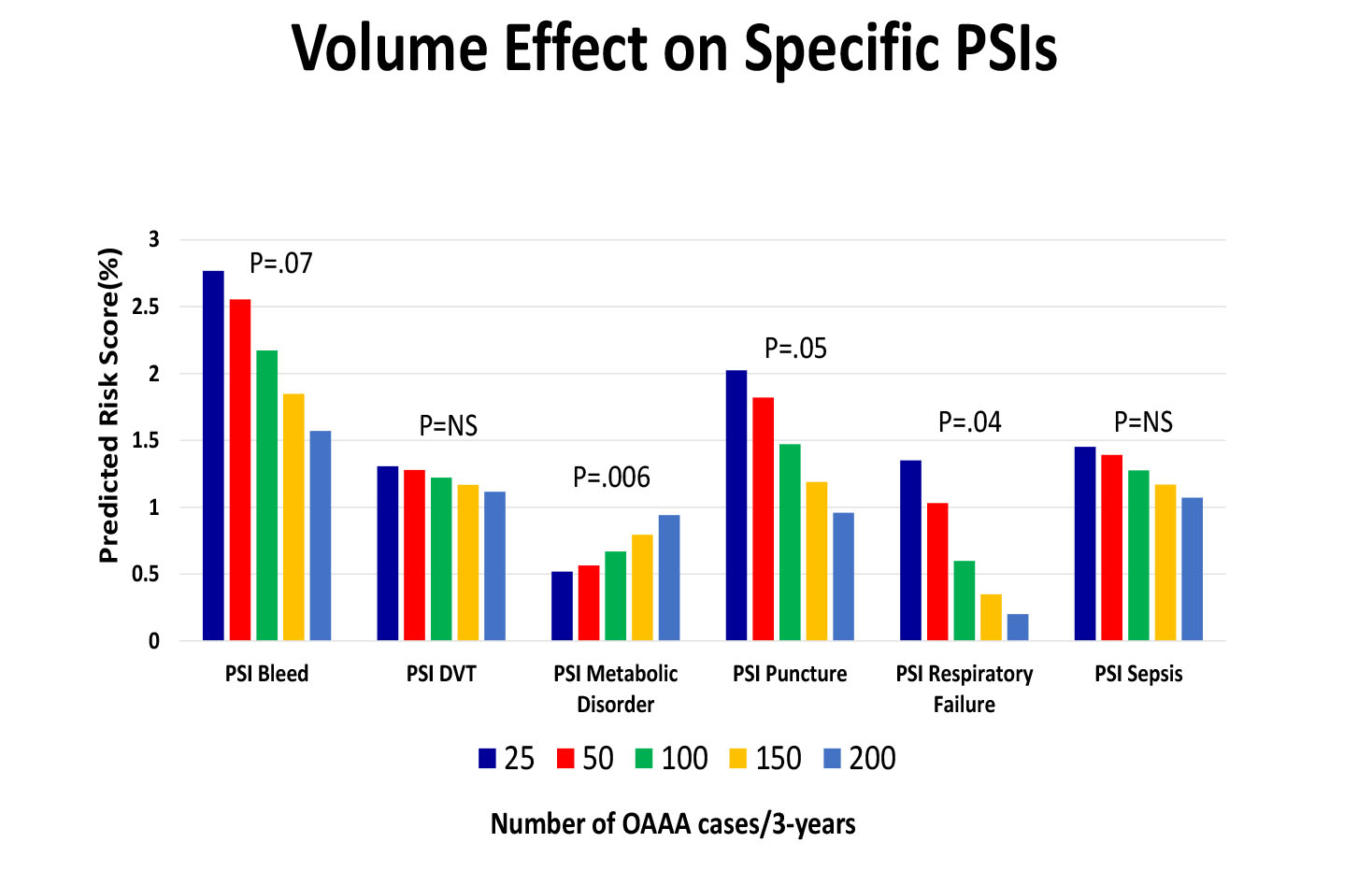
When examining HV effects on the likelihood of developing any complication (45%), PSIs (12%) and FTR (9%), a significant risk reduction was noted in higher volume institutions. Specifically, a non-linear relationship between HV and risk of any complication (P=0.0004), PSI (P=0.0004), and FTR (P=0.0003) was present. When exploring risk of developing specific complication (Figure 1) or PSI events (Figure 2), greater HV was strongly correlated with decreased likelihood of multiple adverse outcomes.
CONCLUSIONS: Although higher volume institutions do not necessarily operate on more comorbid patients, there are important differences in the patients selected for elective repair compared to lower volume hospitals. The risk of developing multiple specific postoperative complications, as well as preventable adverse events preceding FTR is significantly influenced by hospital volume. These findings provide benchmarks for selected quality indicators and further support regionalization of OAAA care. 
Back to 2019 Abstracts
