Great Vessel Revascularization for Anterior Ischemic Optic Neuropathy
Evan R Brownie, Puja Kachroo, J Westley Ohman
Barnes-Jewish Hospital, St. Louis, MO
INTRODUCTION: Vascular surgeons are frequently involved in diagnosing the arteritic form of anterior ischemic optic neuropathy (AION) by performing temporal artery biopsy on the suspicion of giant cell arteritis. Far less frequently do vascular surgeons encounter patients with the non-arteritic form of AION, as there is equipoise between medical and surgical therapies to observation alone. We present a novel case of improvement of AION following complex cerebrovascular revascularization. 
METHODS: The patient is a 61-year-old woman referred by her ophthalmologist for bilateral AION and a chief complaint of declining visual acuity. She is a former smoker who underwent prior right carotid endarterectomy for amaurosis fugax and subsequent left carotid endarterectomy for progression of asymptomatic disease. Her right pupil was nonreactive, and she had no appreciable right upper extremity pulse. Preoperative vascular laboratory studies demonstrated no visualized flow in the right carotid or vertebral systems with antegrade left vertebral flow and a diminutive left carotid. Right upper extremity waveforms were blunted with a diminished forearm/arm index. Computed tomography angiography (CTA) demonstrated a heavily calcified bovine arch origin, a string sign in the left common carotid artery, obliteration of the right carotid system, and a dominant left vertebral artery arising from the left subclavian with minimal orifical disease. Digital subtraction angiography (Figure 1) confirmed CTA findings, as well as an intact Circle of Willis with retrograde distal right vertebral flow and distal right subclavian artery reconstitution. The patient was taken to the operating room with to improve flow to her right posterior and left anterior cerebral circulation. A manubriotomy with left cervical extension was performed to expose the ascending aorta and the cervical left common carotid. The first portion of the right axillary artery was exposed in a standard manner and an infraclavicular tunnel was utilized to link the operative fields. Following systemic heparinization, an ascending aorta to end-to-end cervical carotid arterial bypass was performed with a pre-fashioned jump graft to the right axillary artery utilizing our infraclavicular tunnel (Figure 2). The incisions were closed over a mediastinal drain and the patient was extubated in the operating room. She was transferred to the intensive care unit for the initial perioperative period and discharged from the floor on postoperative day four. 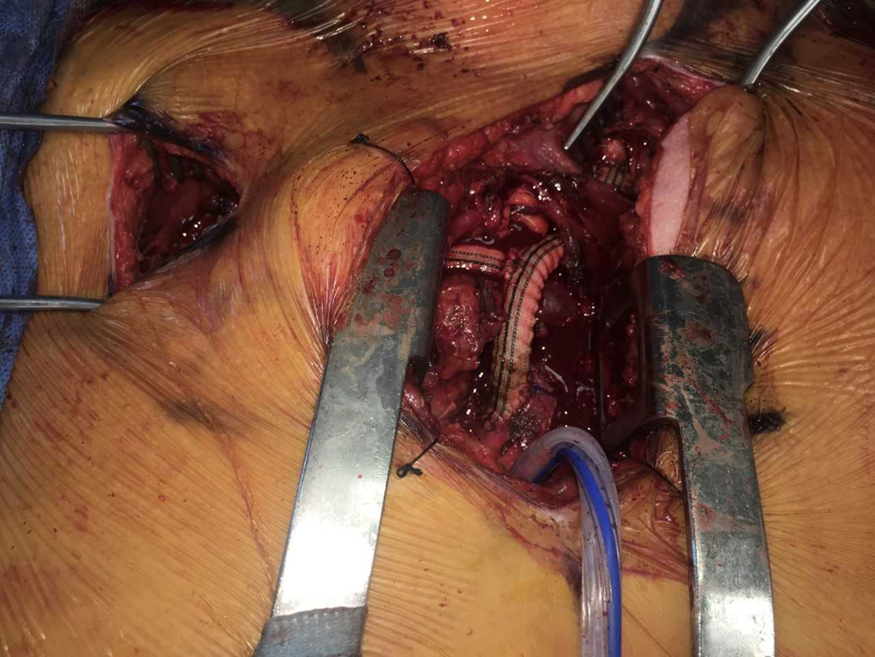
RESULTS: At six-month follow-up, visual acuity in her left eye has improved from 20/400 to 20/20, but she remains blind in her right eye. Physiologic testing demonstrates antegrade bilateral vertebral flow and normalization of her right forearm/arm index in the setting of palpable right upper extremity pulses. Both of her bypass grafts are widely patent on CTA.
CONCLUSIONS: Presented is dramatic improvement of AION following surgical revascularization. This warrants future investigation for operative revascularization non-arteritic AION with occlusive disease of the great vessels.
Back to 2019 Abstracts
