Thoracic Endovascular Aortic Repair in Octogenarians and Nonagenarians: A Single Institution Experience
Akbarshakh Akhmerov, Aamir S. Shah, Ali Azizzadeh
Cedars Sinai Medical Center, LOS ANGELES, CA
BACKGROUND: As a result of improved life expectancy among the elderly, the oldest segments of the population are expanding rapidly. Concurrent with this trend is the increasing number of thoracic endovascular aortic repair (TEVAR) procedures performed in the elderly. Here, we describe our institutional TEVAR experience in octogenarian and nonagenarian patients.
METHODS: All patients ≥ 80 years of age undergoing TEVAR were retrospectively reviewed at a single institution. Patient demographics, preoperative status, operative details, postoperative course, and outcomes were analyzed. Continuous variables are presented as mean ± SD or median [IQR 25th, 75th], and categorical variables are presented as total number and percent.
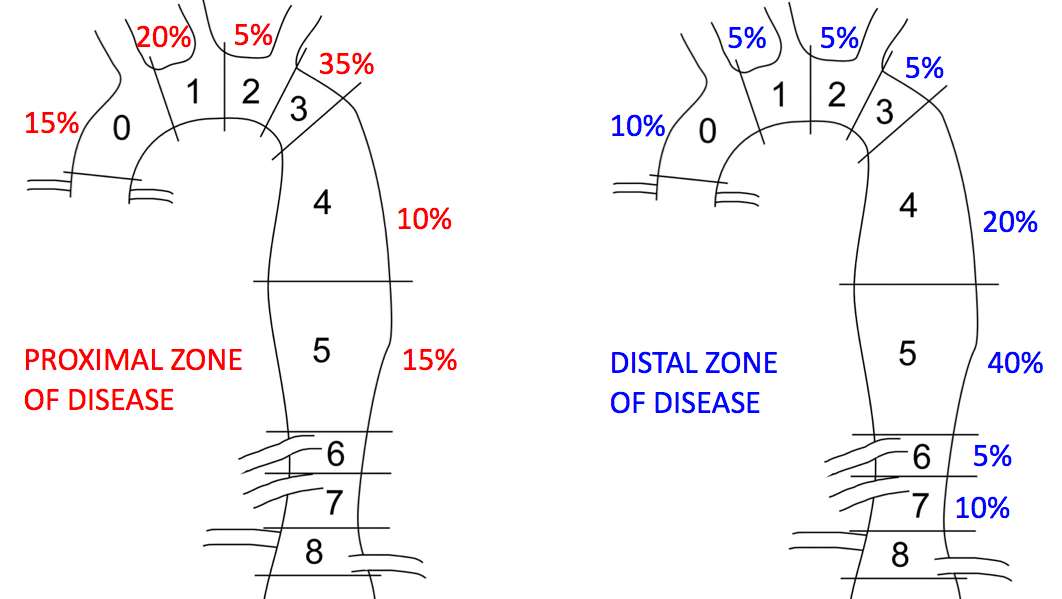
RESULTS: Twenty octo- and nonagenarians (mean age 85.0 ± 3.9 years, 75% male) underwent TEVAR between 2014-2018. In-hospital mortality was 10% (n=2), while overall 30-day mortality was 15% (n=3). Median follow-up was 87 [IQR 19, 249] days. The most common preoperative comorbidities included hypertension (n=19, 95%) and tobacco use (n=17, 85%). Seven (35%) patients had prior aortic aneurysm repairs (endovascular n=5, open n=2). Degenerative aneurysms comprised the majority (60%) of aortic pathologies, with a mean maximal aortic diameter of 63.3 ± 17.0 mm. Zone III was the most common (35%) proximal zone of disease, while zone V was the most common (40%) distal zone of disease (Figure). The mean procedure time was 193.5 ± 125.3 minutes, with most patients requiring one (n=11, 55%), two (n=5, 25%), or three (n=3, 15%) aortic devices. Successful deployment was achieved in 19 (95%) patients; endoleaks were noted in 3 (15%) patients (type II in two patients and type III in one patient). Three (15%) patients experienced postoperative complications, including stroke, arrhythmia, respiratory failure, and congestive heart failure. One patient had an access site injury, which was successfully repaired with a stent graft. ICU length of stay was 2.4 ± 1.9 days, and the total length of stay was 5.3 ± 2.4 days (Table).
CONCLUSIONS: Despite the inherently elevated operative risk among the elderly, this review demonstrates high technical success rate in the octogenarian and nonagenarian populations. Thus, TEVAR is a suitable option for carefully selected elderly patients.
| Extubated in OR | 17 (85%) |
| Lowest Hb (g/dL) | 10.0 +/- 1.5 |
| Vasopressor Use (therapeutic/prophylactic) | 13 (65%) |
| Highest Cr (md/dL) | 1.3 +/- 0.4 |
| Reintervention | 0 (0%) |
| ICU length of stay (days) | 2.4 +/- 1.9 |
| Total length of stay (days) | 5.3 +/- 2.4 |
| In-hospital mortality | 2 (10%) |
| Thirty-day mortality | 3 (15%) |
| Follow up (days) | 87 [19, 249] |
Back to 2019 Posters
