Retrograde Bypass is Preferable to Antegrade Bypass for Open Mesenteric Revascularization
Carlos Huerta, Michael Bounds, Nathan Orr, Eric D Endean
University of Kentucky, Lexington, KY
Background: Despite advances in endovascular surgery, open mesenteric revascularization continues to have a role. Antegrade bypass using the supra-celiac aorta for inflow is the traditional approach. We have modified the technique for retrograde mesenteric revascularization with a direct open retrograde revascularization (DORR) technique. This report is a retrospective, single institution study that describes the DORR technique and compares it to antegrade mesenteric bypass graft.
Methods: Patients undergoing open revascularization between January 2001 and December 2017 for mesenteric ischemia were reviewed. Patients who underwent mesenteric thromboembolectomy, retrograde stenting, or bypass for aneurysmal disease were excluded. Patient demographics, operative details and follow-up data were recorded. Both techniques utilized transabdominal incisions. Antegrade bypasses were constructed using a Dacron graft, exposing the supra-celiac aorta and tunneling graft limbs to the celiac and/or superior mesenteric artery (SMA). DORR was constructed by anastomosing a vein graft to an iliac artery. The vein was tunneled through the base of the small bowel mesentery to create a direct course to the SMA. When revascularization to both the SMA and celiac vessels was indicated, the vein was anastomosed to the SMA in a side-to-side fashion with the distal vein tunneled through the mesocolon and anastomosed end-to-side to the hepatic artery (Image). Student's t-test and Chi square analysis were used with a p0.05 considered significant.
Results: Forty-one patients underwent open mesenteric bypass: 16 antegrade; 25 retrograde. Patient age, gender and BMI were similar. Indication for operation was acute ischemia in a greater portion of patients undergoing retrograde bypass (p=0.015). For antegrade bypasses, Dacron was used in 15 and saphenous vein in 1. The DORR bypass originated from an iliac artery (22), limb of an aorto-femoral graft (2), and infrarenal aorta (1). All DORR were constructed using vein (19 femoral vein, 6 greater saphenous vein). In most DORR configurations, the bypass was created to only the SMA. By comparison, in antegrade bypasses, the bypass was constructed to both the SMA and celiac arteries in all but one (p<0.0001). Operative time was significantly shorter for DORR (307±66 vs. 425±122 min., p=0.007). Blood loss, need for second look laparotomy, morbidity, mortality, LOS and discharge disposition were similar between groups. During the study period, there was a shift in favor of the DORR technique in the second half of the study [2 (15%) DORR from 2001-2009 vs. 21 (81%) DORR from 2010-2017, p=0.0006]. In survivors, 57% of the antegrade cohort and 74% of the DORR cohort had documented follow-up (average 47.5±59.9 months and 28.8±31.3 months, respectively). In both groups, all grafts remained patent.
Conclusions: DORR has become our preferred method for open mesenteric revascularization. The direct tunneling of the graft under the mesentery avoids concern for kinking. This technique has equivalent patency and shorter operative time despite need for vein harvest. The avoidance of prosthetic material makes DORR adaptable for both chronic and acute mesenteric ischemia. 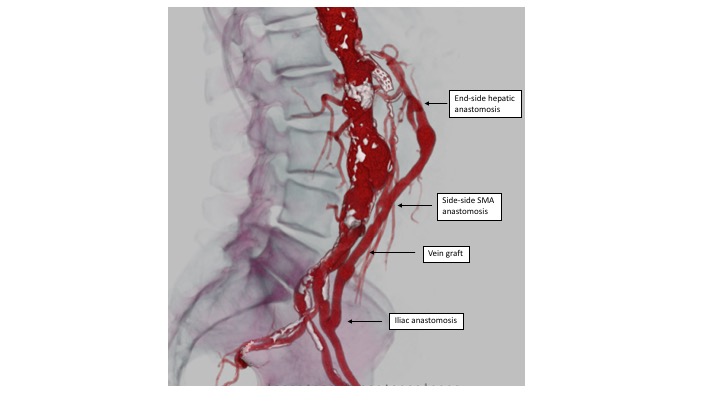
Back to 2019 Posters
