Revascularization of Intermittent Claudicants Leads to Higher Rates of Chronic Limb Threatening Ischemia and Rates of Amputation
Vashisht Madabhushi, Daniel Davenport, Michael Bounds, David Minion, Nathan Orr, Eric Endean, Sam Tyagi
University of Kentucky, Lexington, KY
INTRODUCTION: The US population is aging, and with the aging population there is an increase in incidence of peripheral arterial disease (PAD), The most common symptomatic presentation of PAD is intermittent claudication (IC). The natural progression of symptoms in IC is fairly low at 7-9% the first year and 2-3% each year thereafter, and IC portends an amputation rate of 1-3.3% at 5 years. The progression of IC is mitigated by supervised exercise therapy (SET) and best medical therapy (BMT), but despite the proven benefits of SET and BMT, there has been rapid growth in the invasive treatment of IC. In our healthcare system, PAD is treated by multiple specialties with varying practice patterns, providing an opportunity to investigate disease progression association with treatment strategy. Our aim was to determine if the rate of IC progression to Chronic Limb Threatening Ischemia (CLTI) and amputation rates of patients initially diagnosed with IC were affected by treatment method.
METHODS: This IRB-approved, single center, retrospective study reviewed the records all patients with an initial diagnosis of IC between 6/11/2003 to 4/24/19. Revascularization was defined as endovascular or open. Demographic data was analyzed using descriptive statistics. Time to CTLI diagnosis and amputation were stratified by revascularization status. Multivariate logistic regression was used to analyze demographics and outcomes and propensity matching was used in selecting patients for survival analyses.
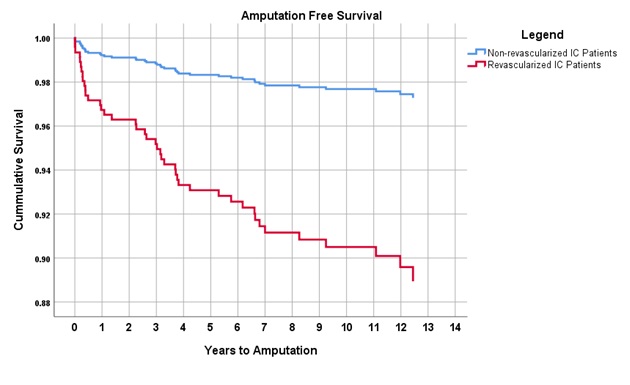
RESULTS: 1137 patients diagnosed with IC were identified. 109 were excluded due to a prior diagnosis of CTLI and 19 were excluded due to revascularization prior to IC diagnosis, leaving 1009 patients. 116 of these patients had at least one revascularization procedure and 893 did not. There was no significant difference in age, smoking status, or comorbidities between the two groups other than the revascularized group had a higher rate of COPD (15% vs. 23%, p <0.05). After risk adjustment, there was a five-fold increase in the progression to CLTI in the revacularized IC group (6% vs. 35%, p <0.001) (Figure 1) and amputation rates were nearly five times higher in the revascularized IC group (3% vs. 14%, p<0.001) (Figure 2). A Cox multivariable regression analysis including age, gender, BMI, DM, COPD, CHF, CKD, and tobacco use, identified revascularization of IC patients to be the significant risk factor for both the progression to CTLI (HR - 6.25, 95% CI 4.01-9.73) and amputation (HR - 6.16, 95% CI 2.83 - 13.42).
CONCLUSIONS: Revascularization of IC patients is associated with an increased rate of progression to CLTI, and increased rate of amputation . While further studies are required to identify which if any IC patients benefit from revascularization procedures. Given the results of this study, we believe that IC patients should be treated with SET and BMT. 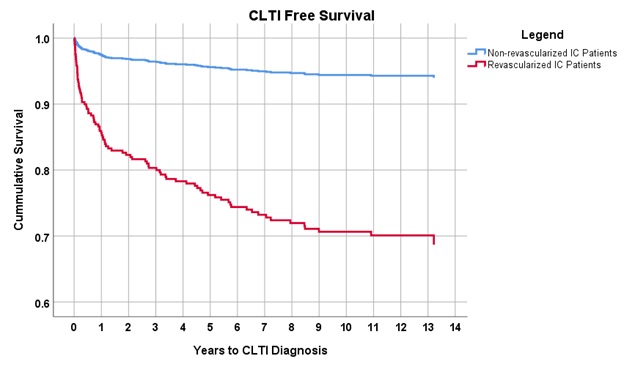
Back to 2020 Abstracts
