Diagnosis and Management of Silent Myocardial Ischemia in Patients Undergoing Carotid Endarterectomy
Dainis K Krievins1, Edgars Zellans2, Andrejs Erglis1, Ligita Zvaigzne2, Roberts Rumba2, Sanda Jegere2, Indulis Kumsars1, Karlis Kaufmanis2, Gustavs Latkovskis1, Christopher K Zarins3
1University of Latvia, Riga, Latvia2Paul Stradins Clinical University Hospital, Riga, Latvia3HeartFlow, Inc, Redwood City, CA
Background: Coronary artery disease (CAD) is the primary cause of death in patients with carotid artery disease and silent myocardial ischemia is a marker for adverse coronary events. Prospective, randomized trial evidence shows that invasive coronary angiography with selective coronary revascularization prior to carotid endarterectomy (CEA) reduces post-op MI and improves long-term survival of CEA patients with no evidence of CAD (Illuminati, EJVES 2015). A non-invasive cardiac diagnostic test, coronary CT and computed fractional flow reserve (FFRCT) can reliably identify ischemia-producing coronary stenosis in stable patients with symptoms of CAD but its value in CEA patients in unknown. We sought to determine the prevalence of silent myocardial ischemia in patients undergoing CEA and to assess the potential value of FFRCT to help guide patient care and improve outcomes.
Methods: Patients with no cardiac history or chest symptoms admitted for elective or urgent CEA were enrolled in a prospective, open label, IRB-approved study and underwent pre-op coronary CT and FFRCT with results available to physicians for patient management. Ischemia-producing coronary stenosis was defined as FFRCT ≤0.80 distal to a focal coronary stenosis. Severe coronary ischemia was defined as FFRCT ≤0.75. Primary endpoint was incidence of major adverse cardiovascular events (MACE, defined as death, MI, stroke or unplanned coronary revascularization) at 30 days with 3, 6 and 12 month follow up.
Results: Coronary CT and FFRCT was performed in 90 consecutive CEA patients (age 68±8 yrs, male 65%, female 35%, hypertension 76%, dyslipidemia 30%, diabetes 10%, smoking 28%). Silent myocardial ischemia was found in 50 patients (56%) with mean FFRCT value 0.71±0.12. Severe coronary ischemia (FFRCT ≤0.75) was present in 38 patients (42%); 28 patients had multivessel ischemia (see Figure). CEA was performed as scheduled in all patients using cardiac anesthesia and close monitoring with no post-op deaths or MIs. All patients received optimum medical therapy and remained free of cardiac symptoms. There were no MACE events at the primary endpoint of 30 days. Based on FFRCT evidence of severe or multivessel myocardial ischemia, coronary angiography was performed in 36 patients, 1-3 months post CEA, with coronary revascularization in 27 patients (23 PCI and 4 CABG; coronary revascularization pending in 5 patients). There have been no complications of coronary revascularization procedures and no MACE events during follow up (74% of patients are at 6 months and 34% at 12 months follow up).
Conclusions: Patients undergoing carotid endarterectomy have a high prevalence of unsuspected, ischemia-producing coronary stenosis which may place them at risk for coronary events. Non-invasive diagnosis with FFRCT can identify patients with increased cardiac risk and help guide patient management. Early results suggest that selective, coronary revascularization
in patients with silent myocardial ischemia may help improve survival, but longer follow up is needed and prospective, controlled trials are indicated. 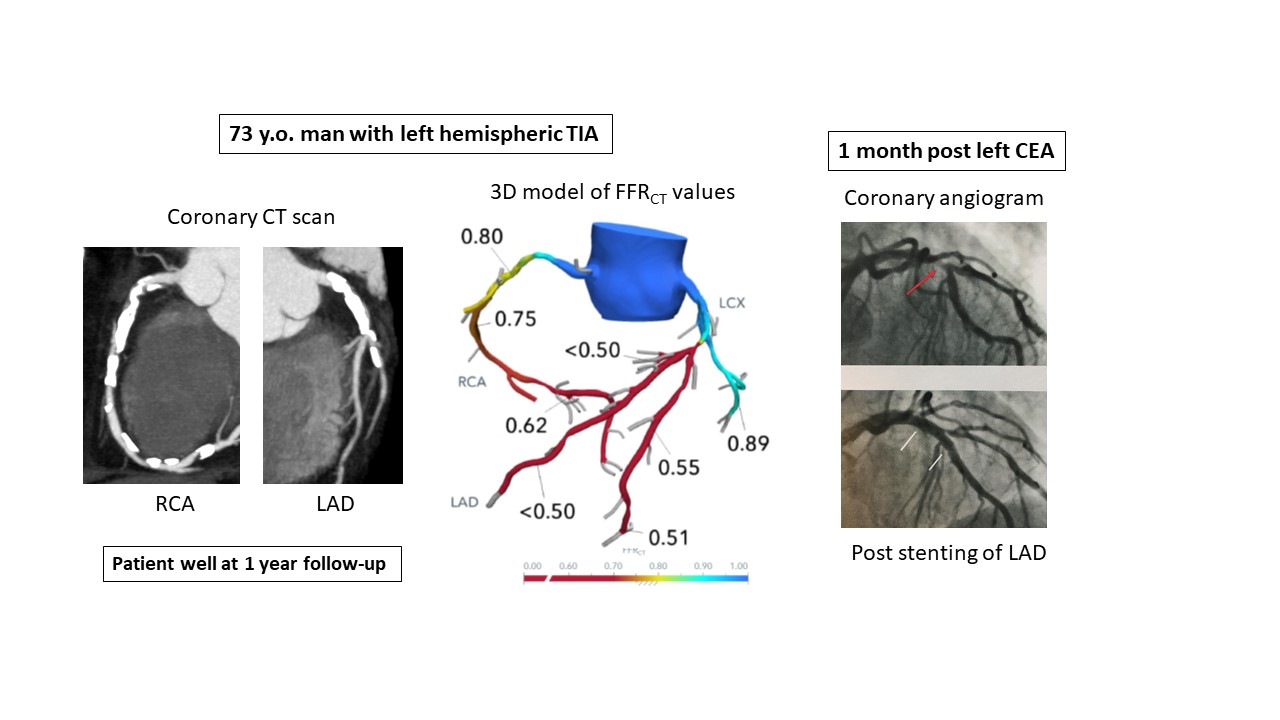
Back to 2020 Abstracts
