Defining the Ninety-Day Cost Structure of Lower Extremity Revascularization for Alternative Payment Model Assessment
Yazan Duwayri1, Francesco A Aiello2, Margaret C Tracci3, Patrick C Ryan4, John G Adams, Jr.5, William P Shutze6, Ying Wei Lum7, Karen Woo8, Robert M Zwolak9
1Emory University, Atlanta, GA;2University of Massachusetts Medical School, Worcester, MA;3University of Virginia, Charlottesville, VA;4Nashville Vascular and Vein Institute,, Nashville, TN;5Columbia Surgical Associates, Columbia, MO;6Texas Vascular Associates, Plano, TX;7Johns Hopkins School of Medicine, Baltimore, MD;8David Geffen School of Medicine at University of California, Los Angeles, Los Angeles, CA;9Dartmouth-Hitchcock Medical Center, Lebanon, NH
Background: The Quality Payment Program is driving Medicare reimbursement to a value-based payment model. The practice of vascular surgery will face significant challenges as a result. The Society for Vascular Surgery Alternative Payment Model taskforce was formed to explore opportunities to develop a Physician Focused Payment Model that will allow vascular surgeons to continue to deliver the complex care of peripheral arterial disease (PAD).
Methods: Medicare beneficiaries undergoing qualifying index procedures during fiscal year 2016 through the third quarter of 2017 were selected for financial analysis. Index procedures were defined using HCPC procedure codes that represent open and endovascular PAD interventions and stratified to inpatient, outpatient and office-based. Inpatient index procedures were included if the procedure code mapped to one of three DRG families consistent with PAD conditions: Other Vascular Procedures (252-254), Aortic and Heart Assist Procedures (268, 269), and Other Major Vascular Procedures (270-272). Patients undergoing outpatient or office-based procedures were included based on HCPC procedure codes. Emergent procedures, end stage renal disease patients, perioperative deaths and patients undergoing interventions in the preceding 30 days were excluded. Analysis captured post-acute care services (PACS) and 90-day Post discharge events (PDE). PACS included rehabilitation, skilled nursing facility and home health services. PDE included emergency department visits, observation stays, inpatient readmissions, and reinterventions.
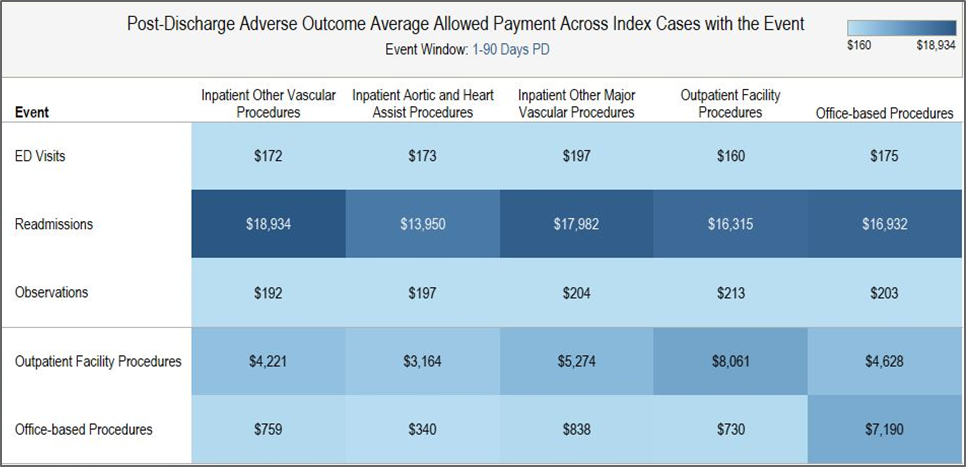
Results: 123,180 cases met inclusion criteria. 82% of cases were performed in the outpatient setting. Inpatient index procedures had a higher cost than outpatient and office-based index procedures. The average cost per index case for DRG (252-254) was $18,755, DRG (268, 269) was $34,600 and DRG (270-272) was $25,245. Average cost was $11,458 for outpatient index procedures and $11,533 for office-based index procedures. PACS were more commonly utilized after inpatient index procedures. Percent PACS utilization and average cost was 58.6% ($5,338), 57.2% ($4,192), and 55.9% ($5,275) for DRG 252-254, DRG 268-269, and DRG 270-272 respectively. Outpatient index procedures required PACS in 13.7% of cases (average cost $1,352) while office-based procedures required PACS in 15% of cases (average cost $1,467). 90-day PDEs were frequent across all sites of service (range 38.9%- 50.2%) and carried significant cost. Readmission was associated with the highest PDE average expenditure (range $13,950- $18.934). The average readmission cost exceeded that of the index procedures performed in the outpatient settings (Tables 1 and 2).
Conclusions: Cost comparisons in PAD interventions should extend beyond the index procedures. Despite analysis challenges related to the breadth of vascular procedures and site of service variability, the data uncovers potential cost saving opportunities in the management of PDE. Due to the vulnerability of the PAD patient population, alternative payment modeling using a bundled value-based approach will require reallocation of resources to focus on longitudinal patient care extending beyond the initial intervention. 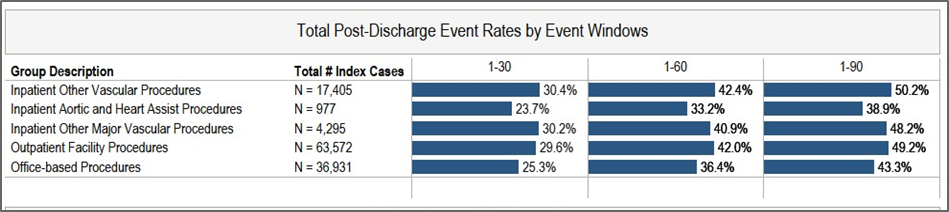
Back to 2020 Abstracts
