The Intricate Association between Case Volume and Years of Practice Experience on Open AAA Repair
Salvatore T. Scali1, Dan Neal1, Kristina A. Giles1, Martin R. Back1, Scott A. Berceli1, Dean J. Arnaoutakis1, Adam W. Beck2, Gilbert R. Upchurch, Jr.1, Thomas S. Huber1, David H. Stone3
1University of Florida, Gainesville, FL;2University of Alabama, Birmingham, AL;3Dartmouth-Hitchcock Medical Center, Lebanon, NH
INTRODUCTION: Widespread adoption of endovascular aneurysm repair has led to a consequential national decline in open aortic surgery (OAR), impacting both vascular surgery trainees and established surgeons alike. While the volume-outcome relationship has been studied extensively, little remains known about the complex interaction of surgeon experience versus case volume on patient selection, procedural characteristics and postoperative complications associated with OAR. The purpose of this analysis was to define the interaction between surgeon years of experience and annual case volume on OAR outcomes.
METHODS: All SVS-VQI infrarenal OARs (n=11,900: elective-71.4%; non-elective-29.6%) from 2003-2020 were examined. Surgeon experience was defined by years in practice after training completion. Experience level at time of repair was categorized chronologically (≤5-years [n=1667], 6-10 years [n=1887], 11-15 years [n=1806], ≥16-years [n=6540]), while annual case volume was determined by the number of OARs performed by the surgeon during the procedure year [median volume=5]. Logistic regression was used to risk-adjust outcomes across experience categories and volume (≤ 5, >5 cases/year) strata for in-hospital major complications, 30-day and 1-year mortality.
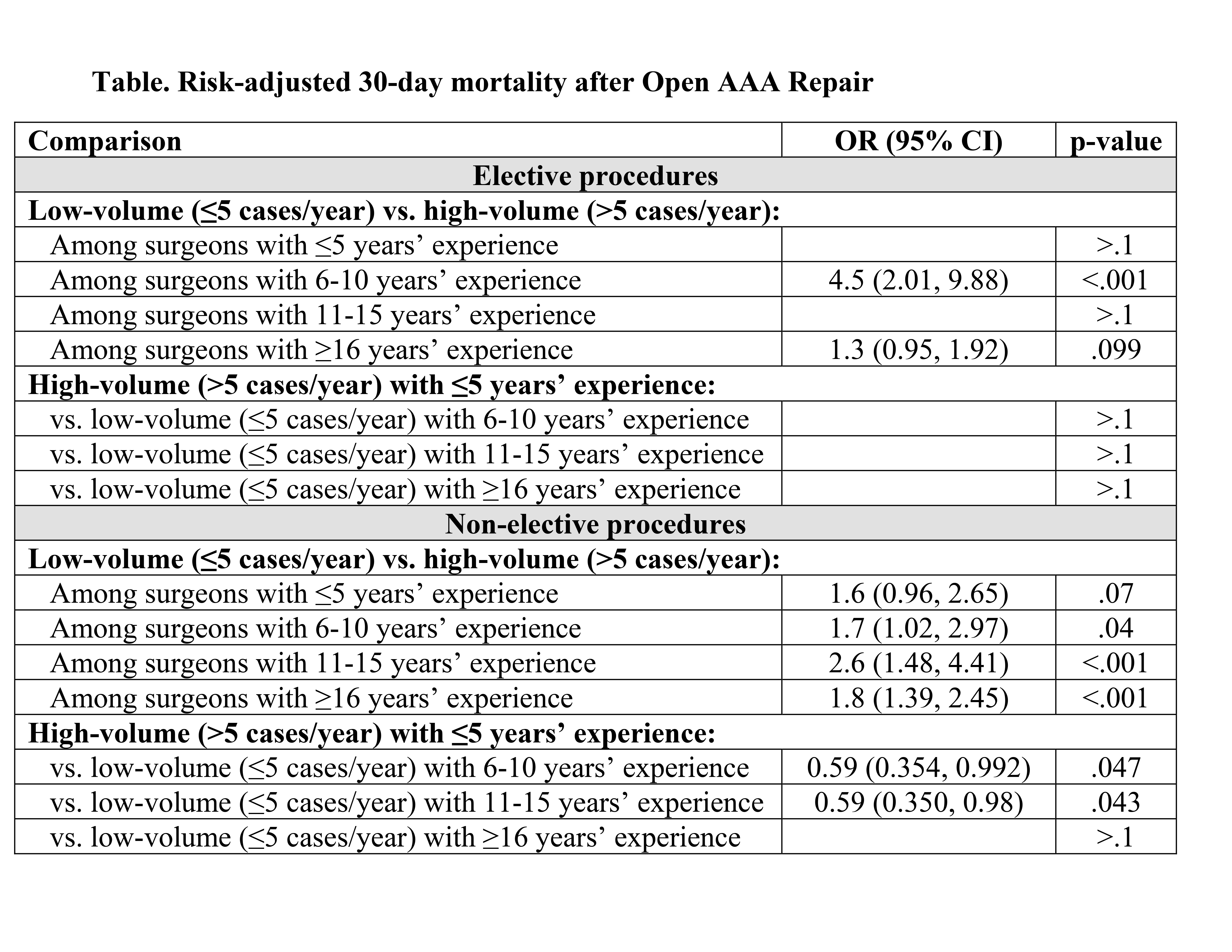
RESULTS: Years in practice (experience) had little effect on unadjusted mortality for elective and non-elective procedures (30-day death: elective P=.2, non-elective P=.3; 1-year death: elective P=.2, non-elective P=.2), although more experienced surgeons had fewer complications after elective OAR (rate for ≥16 years = 25% vs. 29% for ≤5 years, P=.004). However, when surgeons were stratified by case volume and years in practice, surgeons performing >5 cases/year had consistently lower mortality and complication rates for all procedures (Figure). Increasing surgeon experience was significantly associated with performing a greater proportion of elective procedures (Elective: 73%, ≥16-years vs. 62%, ≤5-years; P-trend<.0001) (Non-elective: ≤5-years, 38% vs. 27%, ≥ 16-years; P-trend<.0001). Risk adjustment (model AUC=0.776) revealed that low-volume (<5 cases/year) surgeons had inferior outcomes compared to high-volume surgeons within each experience strata for all presentations (Table). Notably, high-volume, early career surgeons (<5 years) had outcomes similar to older, low-volume surgeons (P>0.1 for all pairwise comparisons). Across experience strata, early career surgeons (<5-years) operated on a greater proportion of elective patients with ASA class 4 designation (34.5% vs. 30.0%, ≥ 16-years; P=.0003) and larger AAA diameters (62±15mm vs. 59±13mm, ≥ 16-years; P<.0001). Use of supra-renal cross-clamp (above 1 or both renal arteries) occurred more frequently (26.2% vs. 22.4%, ≥ 16-years; P=.0009) while total procedure time, estimated blood loss, and renal-visceral ischemia time were all greater for less experienced surgeons (P-trend<.0001).
CONCLUSIONS:Annual OAR case volume appears to be more impactful on OAR outcomes than years of practice experience. To assure optimal OAR outcomes nationally, early practice designation, mentorship strategies for onboarding early career surgeons and low volume aortic surgeons should be considered. These findings have significant implications on widespread initiatives for regulatory and credentialing paradigms. 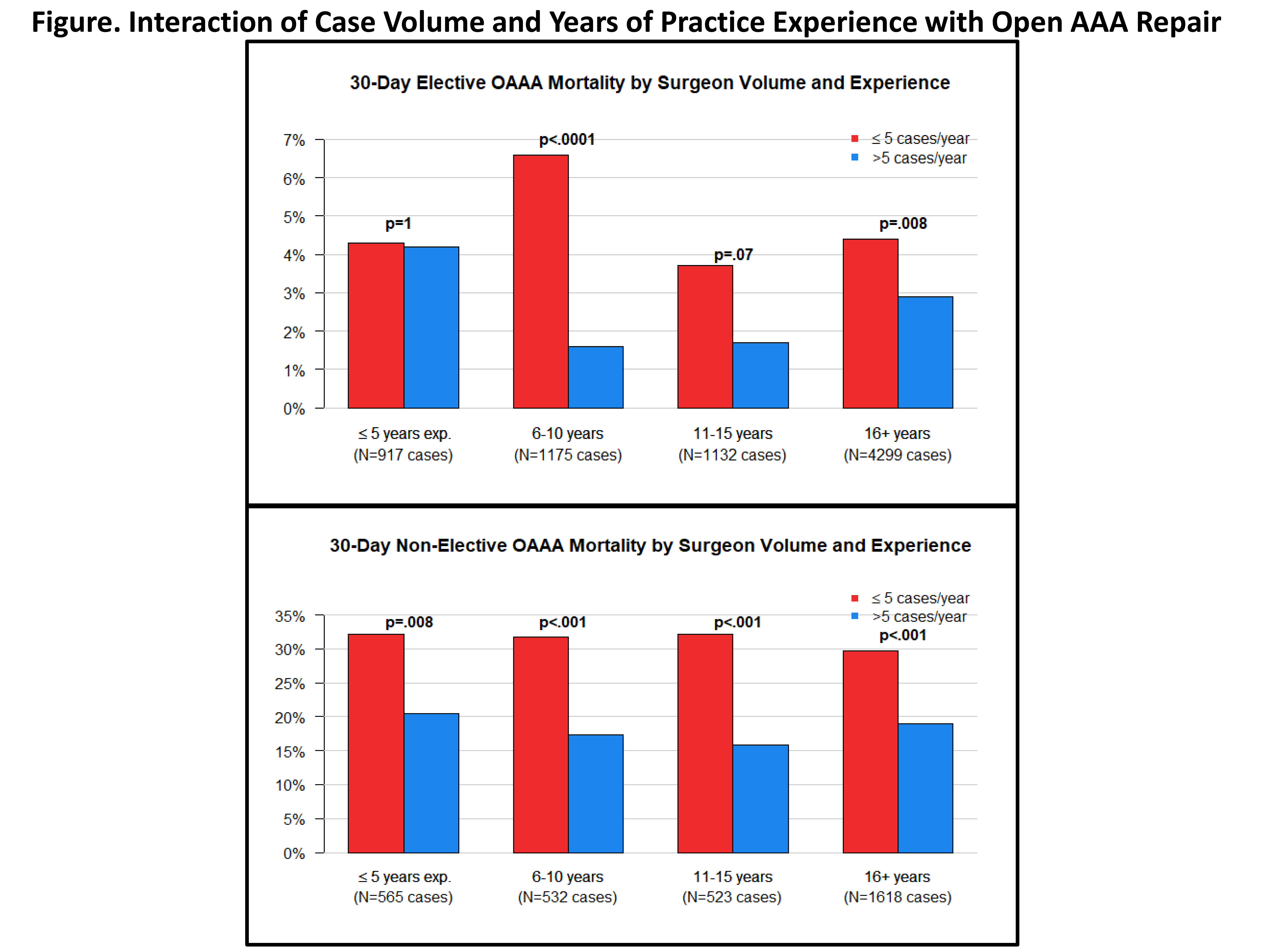
Back to 2020 Abstracts
