ZONE 3 VERSUS ZONE 2 TEVAR FOR ACUTE TYPE B AORTIC DISSECTION: THE CASE FOR A MORE PROXIMAL LANDING ZONE
Tomaz Mesar1, Fanny Alie-Cusson1, Animesh Rathore1, David J Dexter1, Gordon K Stokes1, Jean M Panneton2
1Eastern Virginina Medical School, norfolk, VA;2Eastern Virginina Medical School, Norfolk, VA
INTRODUCTION: Thoracic endovascular aortic repair (TEVAR) has become first line therapy for complicated acute type B aortic dissection (aTBAD). However, the strategy for optimal proximal landing zone (PLZ) remains to be determined. We compared early outcomes and late aortic-related adverse events in patients undergoing TEVAR for aTBAD with endograft deployment in PLZ 2 versus PLZ 3.
METHODS: We performed a retrospective chart review of all adult patients who underwent TEVAR for aTBAD within 6 weeks of diagnosis from January 2008 to December 2018. We excluded patients with connective tissue disorders and prior type A repair. Patients were initially divided into proximal landing zone 2 TEVAR (PLZ2) and zone 3 TEVAR (PLZ3) groups. PLZ2 patients were divided between left subclavian artery (LSA) revascularization (PLZ2R) versus LSA coverage without revascularization (PLZ2C). LSA revascularization was performed via carotid to LSA bypass, transposition or LSA laser fenestration. Groups were compared for need for aortic re-intervention within 36 months of initial admission and freedom from aortic related adverse events and mortality (AREM), defined as need for aortic re-intervention, aortic-related death or aortic rupture.
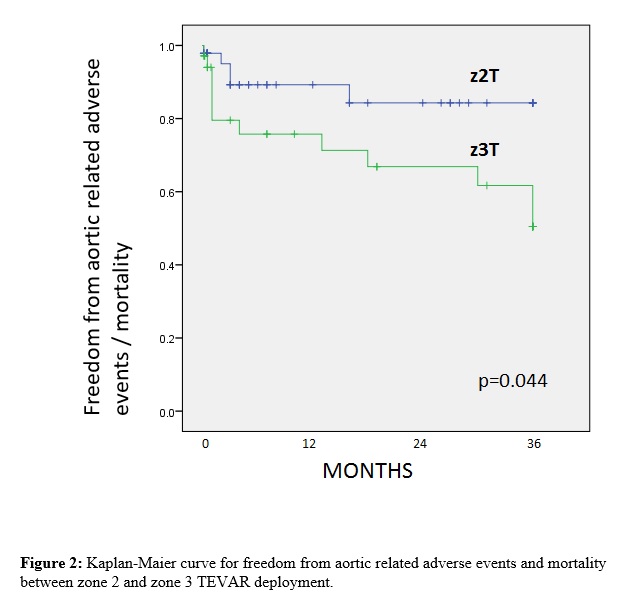
RESULTS: Eighty-two patients underwent TEVAR for aTBAD (mean: 4.1±7.8 days, range: 0-40 days), 35 patients in PLZ3 and 47 in PLZ2; 10 with LSA coverage and 37 with LSA revascularization. There were no differences between PLZ2 and PLZ3 in time from diagnosis to TEVAR, demographics, comorbidities, aortic measurements and operative indications: aortic rupture, 10.4% vs. 11.4% (p=0.910), visceral/extremity malperfusion, 48.9% vs. 34.2% (p=0.185), respectively. 30-day survival was 87.8%: 89.2% for PLZ2R, 85.6% for PLZ3 and 80.0 % for PLZ2C (p=0.612). Stroke rate was 7.2%: 8.1% for PLZ2R, 5.7% for PLZ3 and 10.0% for PLZ2C (p=0.208). Post-operative spinal cord ischemia rate was 3.7%: 2.7 % for PLZ2R, 0% for PLZ3 and 20.0% for PLZ2C (p=0.012). Composite outcome (SCI,stroke or 30-day mortality) was statistically higher for PLZ2C (40.0%) compared to PLZ2R (13.5%), p=0.019. There was no difference in-between PLZ2R and PLZ3, p=0.843. Aortic re-intervention at 36 months post-TEVAR was significantly lower for PLZ2 (8.5%): 2 redo-TEVARs, 1 retrograde type A aortic dissection (rTAAD) and 1 late LSA embolization, compared to PLZ3 (35.4%): 2 rTAADs, 8 redo-TEVARs for endoleak, 1 re-do TEVAR for false-lumen stenting), p=0.027. Post-operative thoracic aortic rupture was 2.2% in PLZ2 and 0 in PLZ3. Freedom from AREM at 36 months was higher in PLZ2 vs. PLZ3 - 89.4% vs. 65.7%, respectively (p= 0.044).
CONCLUSIONS: In patients treated for acute type B aortic dissection, zone 2 TEVAR is associated with a lower need for aortic re-intervention and aortic-related adverse events than zone 3 TEVAR. In our experience, patients may benefit from a more aggressive proximal landing zone with similar and acceptable perioperative morbidity when zone 2 TEVAR is done with LSA revascularization. 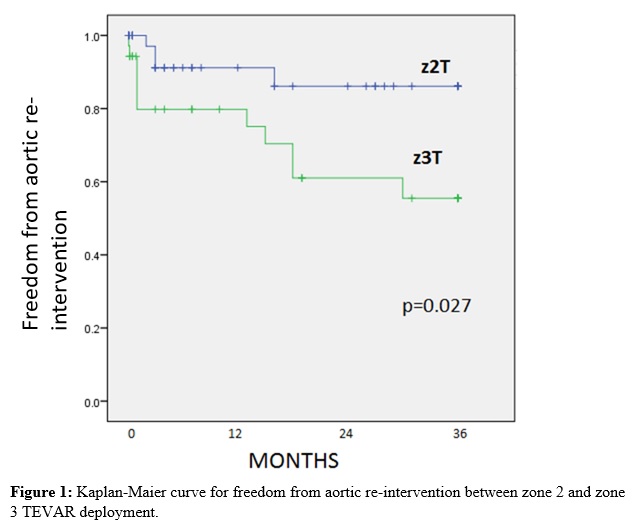
Back to 2020 Abstracts
