Branch Renal Artery Fibromuscular Dysplasia Presenting as Preeclampsia Cured with Second Trimester Balloon Angioplasty
Taylor C Standiford, Gloria Y Kim, Dawn M Coleman, Matthew A Corriere
University of Michigan Health System, Ann Arbor, MI
Background: Associations between preeclampsia and subsequent identification of renal artery stenosis, especially due to fibromuscular dysplasia (FMD), have been previously described. This case report describes a patient without prior history of hypertension who presented during her first trimester with preeclampsia secondary to branch renal artery FMD whose preeclampsia was cured with early second trimester balloon angioplasty. Imaging, medical management, and procedural management details relevant to treating pregnant patients are reviewed.
Methods: a 30-year-old woman without significant past medical history was referred for Vascular Consultation due to severe first trimester preeclampsia with poor blood pressure control with oral antihypertensive medications. Hypertension was identified one week prior to diagnosis of pregnancy, and poorly controlled on high-dose labetolol plus nifedipine. At the time of vascular consultation, the patient had a diastolic blood pressure of 120 mm Hg, headache, and had been evaluated at an Urgent Care Center twice the same week for symptomatic hypertension., and termination of pregnancy was being considered due to maternal risk. A renal artery duplex suggested unilateral distal renal artery stenosis. MRA was performed for anatomic assessment of the lesion, but was performed without contrast due to pregnancy and was negative for hemodynamically significant occlusive disease. The patient was monitored until early second trimester, and then underwent catheter angiography under local anesthesia with pelvic shielding. Angiography confirmed branch right renal artery stenosis consistent with FMD (Figure).
Results: Balloon angioplasty was performed and resulted in immediate post-procedural resolution of preeclampsia. The patient was discharged the following day without need for further oral antihypertensive medications. She delivered a healthy baby at term, and remains normotensive and asymptomatic without need for antihypertensive medications.
Conclusion: Renal artery stenosis may become symptomatic during pregnancy, and should be considered among patients with severe preeclampsia. Non-contrast MRA may produce false-negative results, and contrast angiography should be considered during second trimester in the setting of a positive renal duplex and strong clinical suspicion. Renal angioplasty can be safely performed during pregnancy, with potential cure of preeclampsia in the setting of symptomatic FMD. Although vascular specialists seldom assume primary management of pregnant patients, they should be familiar with principles of medical and procedural management during pregnancy. 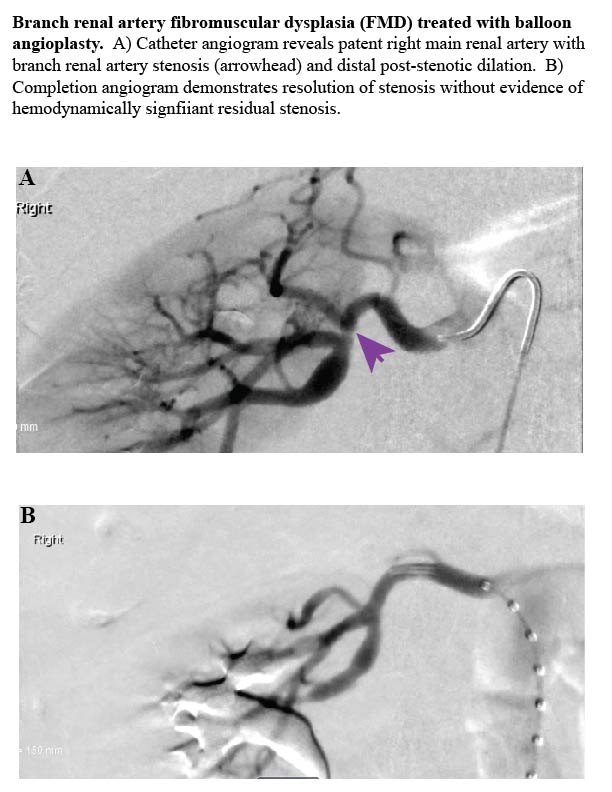
Back to 2020 Abstracts
