Alpha-Gal Syndrome as a Cause for Recurrent Common Femoral Artery Stenosis after Patch Angioplasty with Bovine Pericardium
Ankur Aggarwal1, Allison E Kirkner2, Christopher Moskaluk3, Morgan D Salmon4, Wilson M Jeffrey4, Rung-Chi Li4, Robert B Hawkins2, James A Platts-Mills4, W Darrin Clouse1, Margaret C Tracci1
1University of Virginia, Department of Cardiothoracic and Vascular Surgery, Division of Vascular and Endovascular Surgery, Charlottesville, VA;2University of Virginia, Department of Cardiothoracic and Vascular Surgery, Charlottesville, VA;3University of Virginia, Department of Pathology, Charlottesville, VA;4University of Virginia, Department of Allergy and Immunology, Charlottesville, VA
INTRODUCTION: α-Gal syndrome (AGS) is a disease characterized by delayed hypersensitivity symptoms secondary to the body’s IgE-mediated antibody response to galactose-α-1,3-galactocose (alpha-gal) present in mammalian meat such as beef and pork. In the United States, the disease is linked to host antigens delivered through the bite of the lone star tick, amblyomma americanum, with a range comprising the Southeast, lower Midwest, and Eastern United States (Figure 1). The incidence of reported AGS is rising worldwide and in the United States specifically, it is heavily concentrated in the Southeast. We present the first report in the literature of a clinically significant, immunologically confirmed case of AGS associated with failure of a common femoral artery patch angioplasty, using bovine pericardium as the patch material, requiring reoperation. METHODS: The index patient was treated for acute bilateral iliofemoral occlusion and underwent bilateral iliac and lower extremity thromboembolectomy, fasciotomy, and femoral endarterectomy with patch closure utilizing bovine pericardium (XenoSure®, LeMaitre Vascular™). At 1 month followup, a history of food allergy to beef was elicited. Subsequently, the patient developed severe, symptomatic restenosis of the femoral arteries, comfirmed by ultrasound and CT angiography, requiring revision. At re-operation, an intense local inflammatory response surrounding the artery was noted. The patch was replaced with woven polyester (Dacron®, Vascutek™). Based on clinical suspicion due to the beef allergy and unusual clinical course, the patient was tested for AGS and the explanted graft sectioned for both standard pathological evaluation and for immunohistochemistry. RESULTS: Evaluation by the Department of Allergy and Immunology confirmed the diagnosis of AGS with elevated IgE (391 IU/ml) and sIgE (76 kU/L) levels. Pathological examination of the resected specimen noted the explanted pericardial tissue displayed a dense fibrous nature consistent with focal foreign body inflammatory reaction. Immunofluorescent microscopy revealed positive staining for antibodies consistent with the alpha-gal epitope. CONCLUSIONS: Bovine pericardium is a widely utilized graft material in vascular surgery, thought to be useful based on its availability, handling characteristics, and relative resistance to infection. However, the increasing incidence of AGS, particularly in the Southeastern United States raises the possibility that patients with preexisting sensitization may be prone to graft failure, underscoring the importance of food allergy in the patient history. In addition, a report in the cardiac surgery literature suggests an association between failure of bioprosthetic (porcine) valves and AGS in patients who were presumed to have acquired the exposure and sensitization post-implantation. There have also been reported associations between AGS and anaphylactic reactions to certain drugs and one report of an intraoperative anaphylactic reaction after exposure to a topical hemostatic agent (Surgiflo®) containing porcine gelatin. We recommend careful evaluation of preexisting allergies and consideration of potential exposure when selecting mammalian bioprosthetics for use in vascular surgery. 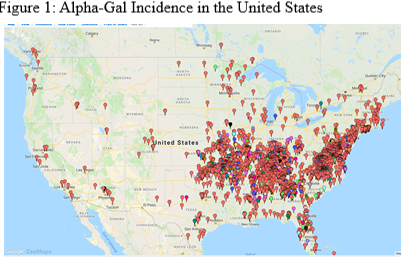
Back to 2020 Abstracts
