Endovascular Management of Penetrating Carotid Trauma with Flow Diverting Stents
Jaime Benarroch-Gampel, Diogo C Haussen, Ravi R Rajani
Emory University School of Medicine, Atlanta, GA
BACKGROUND: While flow diverting stents have previously been described for the treatment of intracranial aneurysms, their use in the management of traumatic vessel injury has been limited. We present an index case of a patient with a pseudoaneurysm of the internal carotid artery (ICA) after a gunshot wound who underwent endovascular repair with a flow diverting bare stent.
METHODS: The patient is a 33-year-old male who presented after multiple gunshot wounds to the left face. Initial computed tomography angiogram (CTA) of the neck and face was obtained which revealed the presence of thrombus in the right ICA 3.5cm above the bifurcation. He was started on antiplatelet therapy and remained without neurological deficits. On follow up CTA, he was found to have a 2.7cm pseudoaneurysm arising from the injured segment of the ICA (Image 1). Due to the small size of the vessel and its tortuosity, the decision was made to treat the lesion with a flow-diverting stent. After common femoral access was obtained, selective catheterization of the right common carotid artery was performed. The injured segment of the ICA was crossed with a microcatheter to the petrous portion of the ICA. At this point, a flow diverting stent (Pipeline Flex® 5mm x 35mm embolization device, Medtronic, Minneapolis) was inserted and deployed across the pseudoaneurysm. Due to severe tapering of the vessel, the proximal portion of the flow diverting stent was reinforced with a self-expanding uncovered stent (Xact®, Abbot, Illinois). Completion angiogram revealed near-complete resolution of the pseudoaneurysm. Postoperatively, the patient remained neurologically normal and was discharged on the first post-operative day on dual antiplatelet therapy.
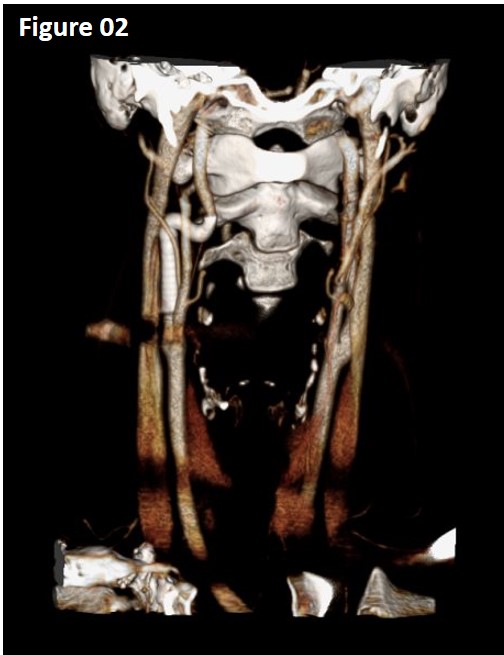
RESULTS: The patient was last seen 7 months after the intervention. He has no neurological symptoms. He remains on single antiplatelet therapy with aspirin as Plavix was discontinued on his previous clinic visit 5 months after the intervention. Follow up CTA demonstrated resolution of the pseudoaneurysm and patent stents without abnormalities (Image 2).
CONCLUSION: We here describe the first case reported in the literature using a flow diverting stent for the management of an ICA pseudoaneurysm following penetrating trauma. Flow diverting stents should be considered a valuable option for the endovascular management of these patients, particularly when treating small diameter or tortuous vessels. 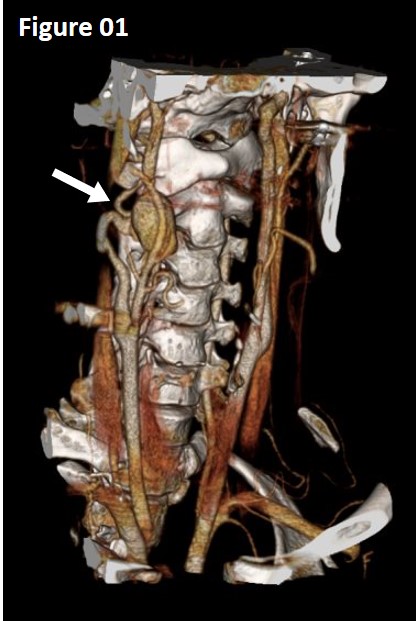
Back to 2020 Abstracts
