Rapid Progression of Carotid Stenosis is Rare in a Large Integrated Healthcare System Over an Eight-Year Period
Carney Chan, Daniel Fort, Cruz Velasco-Gonzalez, Ryan Bedi, Thomas N Hawken, Charles C Leithead, Clayton J Brinster, Waldemar C Sternbergh, III, Hernan A Bazan
Ochsner Clinic, New Orleans, LA
BACKGROUND: Current Society for Vascular Surgery guidelines suggest screening for asymptomatic carotid stenosis in a select group of high-risk patients with certain risk factors. Previously, The Asymptomatic Carotid Stenosis and Risk of Stroke study followed 1,121 patients with >50% stenosis for a mean of 4 years and found some degree of carotid stenosis progression in 19.8% of patients. While these studies examined the natural progression of carotid stenosis, there is a paucity of data on rapid progression of carotid stenosis on a large scale. As hospitals and health systems increasingly rely on Electronic Medical Records (EMR), physicians are able to utilize some of its inherent capabilities, such as the capacity to instantly share patient information between multiple remote hospitals. Another benefit of EMR is the ability to access a large patient database with pertinent data from multiple discrete specialties, such as sequential carotid duplex ultrasounds ordered by primary care physicians. Although this type of information has been available for years, carotid stenosis is the result of expert interpretation of several key measurements and often requires additional commentary to support and contextualize findings. This presented a new challenge, as unlike simple lab results, ultrasound reports were frequently provided in a number of different formats, often with the degree of stenosis buried in a paragraph. In order to extract and analyze carotid stenosis levels, we created a custom software algorithm that allowed analysis of an electronic dataset of over 4 million patients. Using this novel algorithm, we aimed to examine the natural progression of carotid stenosis over time, identify a subset of patients with rapid progression of carotid stenosis, and evaluate specific patient risk factors associated with this rapid progression of carotid stenosis.
METHODS: Patients in a large integrated healthcare system who received two or more carotid duplex ultrasounds for carotid stenosis from August 2010 to August 2018 were identified. An algorithm was created to identify which patients displayed rapid progression of carotid stenosis and also to determine associated patient risk factors and co-morbidities. We first queried an electronic data warehouse containing over 4 million unique patients for all available carotid ultrasounds performed in Intersocietal Accreditation Commission-accredited vascular labs, using appropriate EMR ordering codes for each specialty: vascular surgery, cardiology, and radiology. Although our current EMR (Epic Systems Corporation, Verona, WI) was not implemented until 2011, vascular ultrasound results preceding this time are available for view in our system, with reports saved and coded as multi-line “lab results.” Next, the texts of the ultrasound interpretations were retrieved and reassembled for all patients, then filtered to retain only patients with two or more ultrasound examinations. We then created a custom software algorithm using Python 2.7.10 to process the text of these reports. Reports were initially parsed to identify and extract the “Findings,” “Impression,” or “Recommendations” sections. These subsections were broken into sentence and clause chunks. Finally, the chunks were analyzed to determine whether they referenced carotid stenosis. Left or right laterality was identified and any mention of the level or degree of stenosis was extracted. The results then underwent multiple rounds of validation to ensure that the data was accurate. Individual patient data points were manually checked and compared to the algorithm results. If any discrepancies were noted, the algorithm was revised, and the process repeated until no further discrepancies were found. These degrees of stenoses were then categorized into levels 1 through 5: Level 1, 0-39%; Level 2, 40-59%; Level 3, 60-79%; Level 4, 80-99%; Level 5, complete
occlusion. In case the degree of stenosis did not cleanly fall into one of these categories, the patient was classified by the highest mentioned degree. Demographics and clinical characteristics potentially contributing to carotid stenosis were collected on all patients. The primary endpoint was rapid versus slow progression of carotid stenosis. “Rapid progression” was defined as an increase of two or more levels within 18 months and slow as anything outside that parameter. The association of demographic and clinical characteristics with progression of carotid stenosis was assessed by univariate and multivariate logistic regression with Firth correction to address potential data sparseness. The multivariate model was developed by including main linear effects of all covariates available and subject to a liberal alpha=0.2 to remain in model by backward selection. Unadjusted and adjusted odds ratios (OR) and corresponding 95% confidence intervals were obtained. Analyses were carried out in SAS STAT 14.2.
RESULTS: With an initial cohort of over 4 million patients, the algorithm identified 4,982 patients with two or more duplex ultrasounds over an eight-year period, from August 2010 to August 2018. This identified 10,037 carotid arteries that underwent 29,363 ultrasounds, for a mean of 2.9 ultrasounds per carotid. Median follow-up was 31.1 months (0.1 – 93.7 months). Over the course of the study, 4,103 (82.4%) patients did not show any progression, while 879 (17.6%) patients had some level of progression. We found 639 (12.8%) patients progressed 1 level, 164 (3.3%) 2 levels, 50 (1%) 3 levels, and 26 (0.5%) progressed 4 levels. Of those that progressed, 116 (2.3%) progressed to level 4 (80-99% stenosis) from any starting level, over a median time of 11.5 months, with an average starting level of 2.1 (40-59% stenosis). Additionally, 41 patients progressed from level 3 to level 4 overall, while 37 patients progressed from level 3 to level 4 within 18 months. A total of 180 (3.6%) patients were identified as “rapid progressors” (Figure), with a progression of 2 or more levels within 18 months. Median follow-up time was 9.9 months. Final multivariate analysis (Table) showed that younger age (P<0.01), Caucasian race (P=0.02), lower BMI (P=0.01), a diagnosis of peripheral arterial disease (PAD) (P=0.03), and a diagnosis of transient ischemic attack (TIA) (P<0.01) are associated with rapid progression.
CONCLUSIONS: A minority of patients demonstrated rapid progression of carotid stenosis in a population of over 4 million patients over an eight-year period. To our knowledge, this is the largest series to date evaluating the natural progression of carotid stenosis. Our dataset included all patient ultrasounds performed in an integrated health system, not just those ordered by vascular surgeons or other interventionalists. We found that of the 4,982 patients with multiple carotid ultrasounds, 17.6% (879) showed some degree of progression, which is consistent with prior studies, but only 3.6% (180) were rapid progressors. We identified younger age, Caucasian race, lower BMI, diagnosis of PAD, and diagnosis of TIA as risk factors for rapid progression. In those that showed any level of progression, 20.5% were rapid progressors. Thus, while the overall incidence of rapid progression is low, those who demonstrate any degree of progression may warrant closer follow-up, especially if they have the associated risk factors for rapid progression. Lastly, while EMR has been linked with physician burnout, we demonstrated a positive and novel use of this technology to understand the natural history of diseases, as this approach could be applied for other disease processes. We created a custom software algorithm that can be utilized to extract data from reports
written out in paragraph form in a number of different formats. This creates the ability to efficiently and effectively convert text into data points, making it possible to examine large patient datasets that in the past would have been prohibitively large, due to requiring manual review and entry into a database. Future directions include analyzing our current data to predict which patients will undergo rapid progression of carotid stenosis, as well as adapting the custom software algorithm to examine other disease processes. 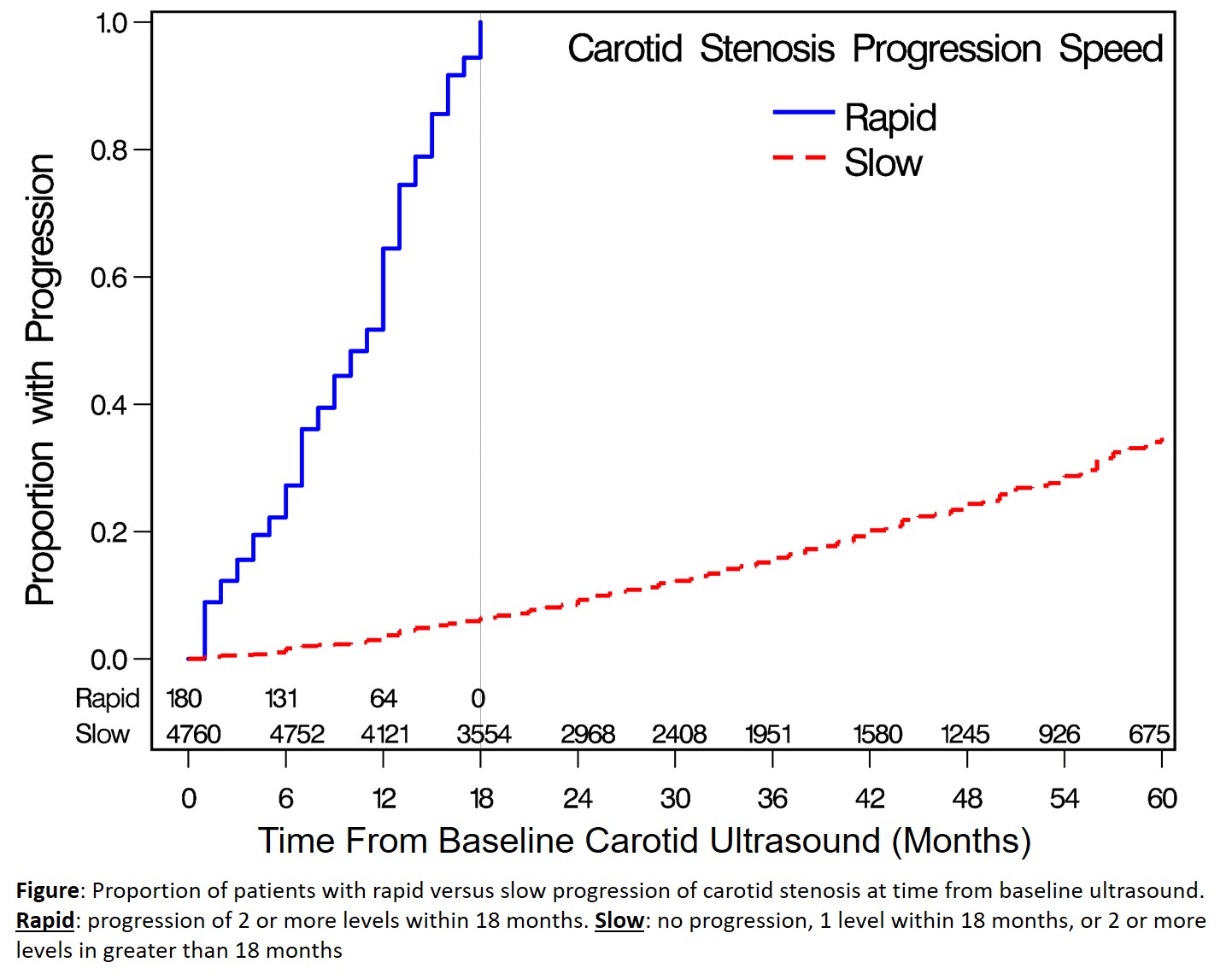

Back to 2020 Abstracts
