Carotid-subclavian bypass for left arm ischemia due to a right sided aortic arch with isolated left subclavian artery
Elizabeth H Weissler, James H Ronald, Cynthia K Shortell, Chandler H Long
Duke University, Durham, NC
BACKGROUND: PD presented with four years of worsening activity-related left neck and arm pain with paresthesias in her first three fingers on the left side. Her pain limited her activities of daily living. She denied dizziness, coordination difficulties, or a history of structural heart disease. Exam revealed left arm weakness, diminished motor function of her left upper extremity, and a 30mmHg brachial pressure differential. MRI showed a right sided aortic arch with an isolated left subclavian artery. Angiogram revealed that her left subclavian and left vertebral arteries were supplied by a paravertebral collateral, with retrograde left vertebral artery flow during left arm abduction. Duplex ultrasound demonstrated monophasic left subclavian flow at 91cm/s compared to 150cm/s on the right. She subsequently underwent left carotid-subclavian bypass with a 6mm ringed PTFE graft. She recovered uneventfully. Her left arm pain and paresthesias resolved and she regained a significant amount of strength in her left arm. 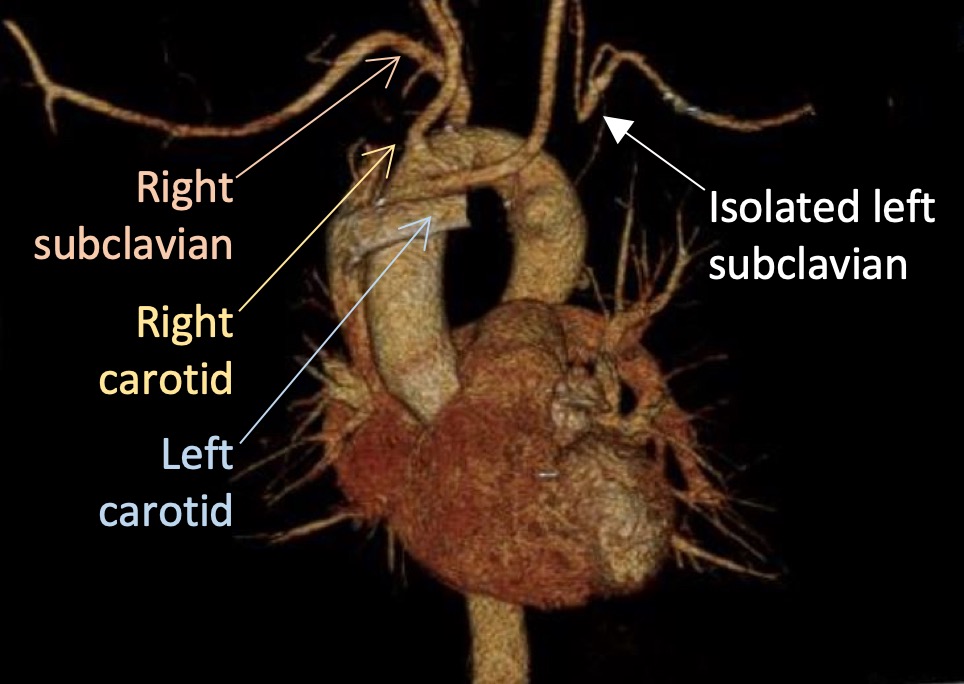
METHODS: PubMed was searched for reports of right-sided aortic arch (RAA) with isolated left subclavian artery (ILSA), whether operatively repaired or not. All available papers in English were reviewed.
RESULTS: Typical great vessel branching from a left sided aortic arch is seen in only 70-80% of the population. RAA is present in 0.05-0.10% of the population. The left subclavian can become “isolated” in RAA: it arises from the ductus arteriosus or ligamentum arteriosum rather than the aorta. This is caused by arch regression in two places: between the left common carotid and left subclavian and distal to the left subclavian. In RAA with ILSA, the first branch is the left common carotid, then the right common carotid and right subclavian. More than half the time, this is associated with congenital heart disease (CHD, usually tetralogy of Fallot).
Most reports of RAA with ILSA are in children, including some reports of children with underdeveloped left arms who have benefitted from subclavian reconstruction during CHD correction. Less frequently does RAA with ILSA cause symptoms in adults. This is much less commonly associated with CHD. Luetmer and Miller published a classic case report and review of RAA with ILSA in 1990, at which time there were 13 cases reported in adults, of whom eight were symptomatic (three with vertebrobasilar insufficiency, three with left arm ischemia, and two with both). There have been few reports of operative repair of RAA with ILSA in adults, and none have been reported in the contemporary era. More recently there have been three separate case reports of conservative management in inidividual adult patients.
CONCLUSIONS: RAA with ILSA is rare. As cross-sectional imaging becomes increasingly frequent, incidental findings of RAA with ILSA may become more common. Knowledge of its etiology and pathophysiology are important for both conservative and operative management. We report the first repair of RAA with ILSA in the contemporary era in a patient with severe left upper extremity ischemia.
Back to 2020 Posters
