Utility of Neuromonitoring in Thoracic Endovascular Aortic Repair - Listening through the Noise
Christian V Ghincea, Adam M. Carroll, Leighton T. McCabe, Kaitlin Roth, Kelly Aunkst, Muhammad Aftab, T. Brett Reece
University of Colorado, Denver, CO
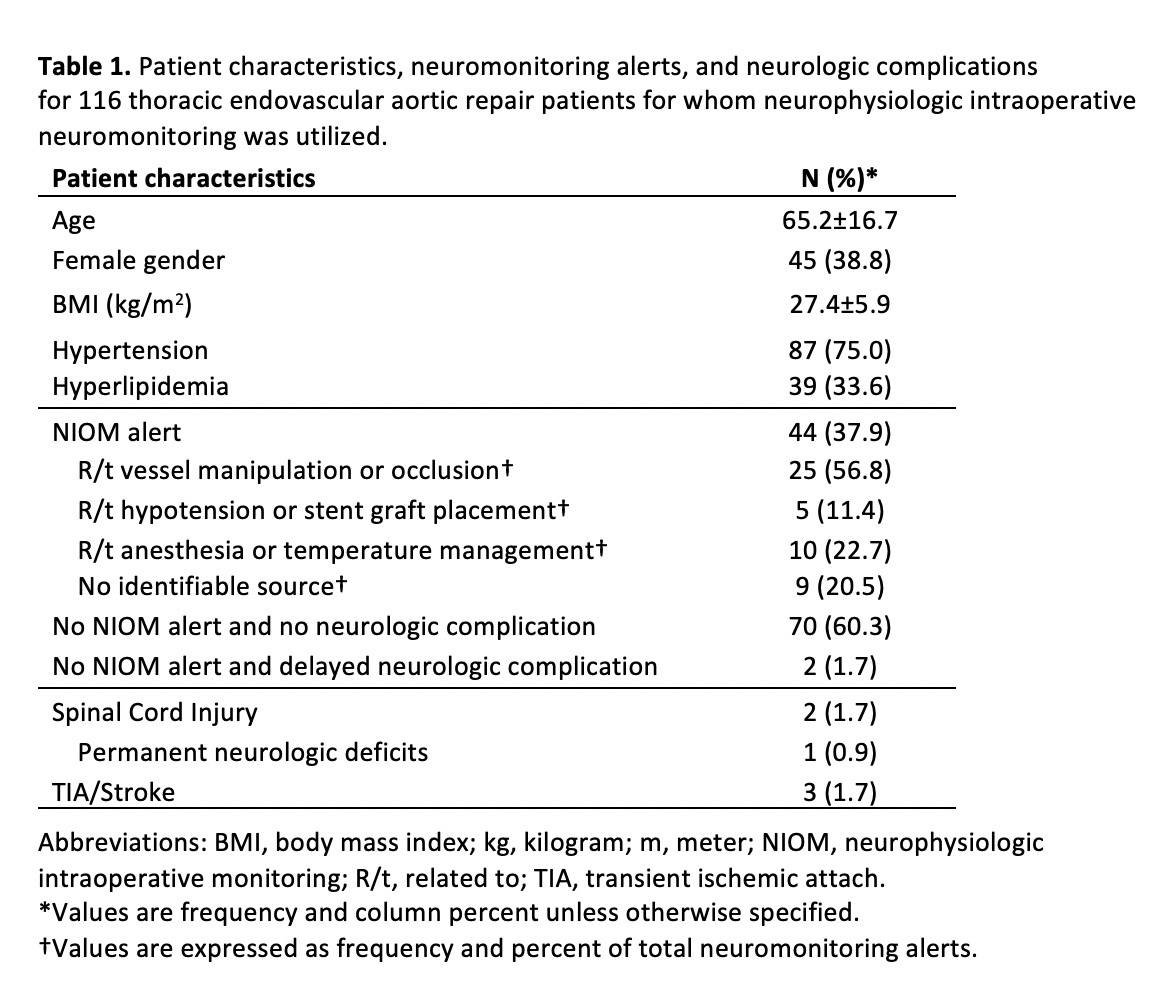
INTRODUCTION: Spinal cord injury and stroke remain potentially devastating complications of thoracic aortic intervention. Neurophysiologic intraoperative monitoring (NIOM) is often used to guide neuroprotective strategies, but the modality has been criticized for a high rate of false positive alerts. Many NIOM abnormalities return to baseline without intervention, making the noise difficult to discern from true complications. The purpose of this study was to evaluate the nature of NIOM alerts during thoracic endovascular aortic repair (TEVAR) and the effectiveness of NIOM for the early detection of neurologic complications. METHODS: We identified 235 patients who underwent TEVAR over 13 years. Of these, 116 cases utilized NIOM, which included somatosensory evoked potentials and motor evoked potentials. For this cohort we reviewed the incidence and timing of spinal cord injury (SCI), the incidence, timing, and location of strokes, and the incidence and nature of NIOM alerts. The patient selection process is described in Figure 1. RESULTS: Table 1 summarizes patient characteristics, neuromonitoring alerts, and neurologic complications for the 116 patients who underwent TEVAR with NIOM. NIOM alerts were documented in 44/116 cases (37.9%). Of the neuromonitoring alerts, 25 (56.8%) were related to arterial manipulation or occlusion, including stent graft delivery sheath placement, dissection, and manual compression. In 10/44 cases (22.7%) NIOM alerts correlated to administration of anesthesia medications or core body temperature cooling, and 5/44 alerts (11.4%) resulted from hypotension or stent graft deployment. For 9/44 patients (20.5%) no intraoperative cause was identified for the NIOM alerts. One of these 9 patients (0.9% of the entire cohort) was diagnosed with a small right superior cerebellar artery stroke on postoperative day 1 after having persistent symptoms of vertigo though no motor or sensory deficits were noted on exam. Regarding other neurologic complications, 1 patient (0.9%) had a transient ischemic attack with right upper extremity weakness on postoperative day 1, 1 patient (0.9%) had delayed SCI on postoperative day 3, and 1 patient (0.9%) developed SCI and right basal ganglia hemorrhagic stroke≥2 weeks postoperatively. Besides the patient with vertigo and cerebellar stroke, one of the remaining 3 patients with neurologic complications had a NIOM alert that did not correlate to exam deficits, and 2 did not have alerts. However, the 2 without alerts presented with delayed neurologic symptoms, so NIOM would not detect these complications. CONCLUSIONS: In conclusion, despite a high false positive rate of alerts, NIOM facilitates the intraoperative detection of vascular and neurologic abnormalities, rather than waiting for postoperative exam deficits, and can lead to timely intra- and post-operative interventions to reverse deficits and improve outcomes. In this cohort, no patients developed spinal cord ischemia immediately postoperatively. Further study is needed to determine the utility of NIOM for the early detection of stroke. 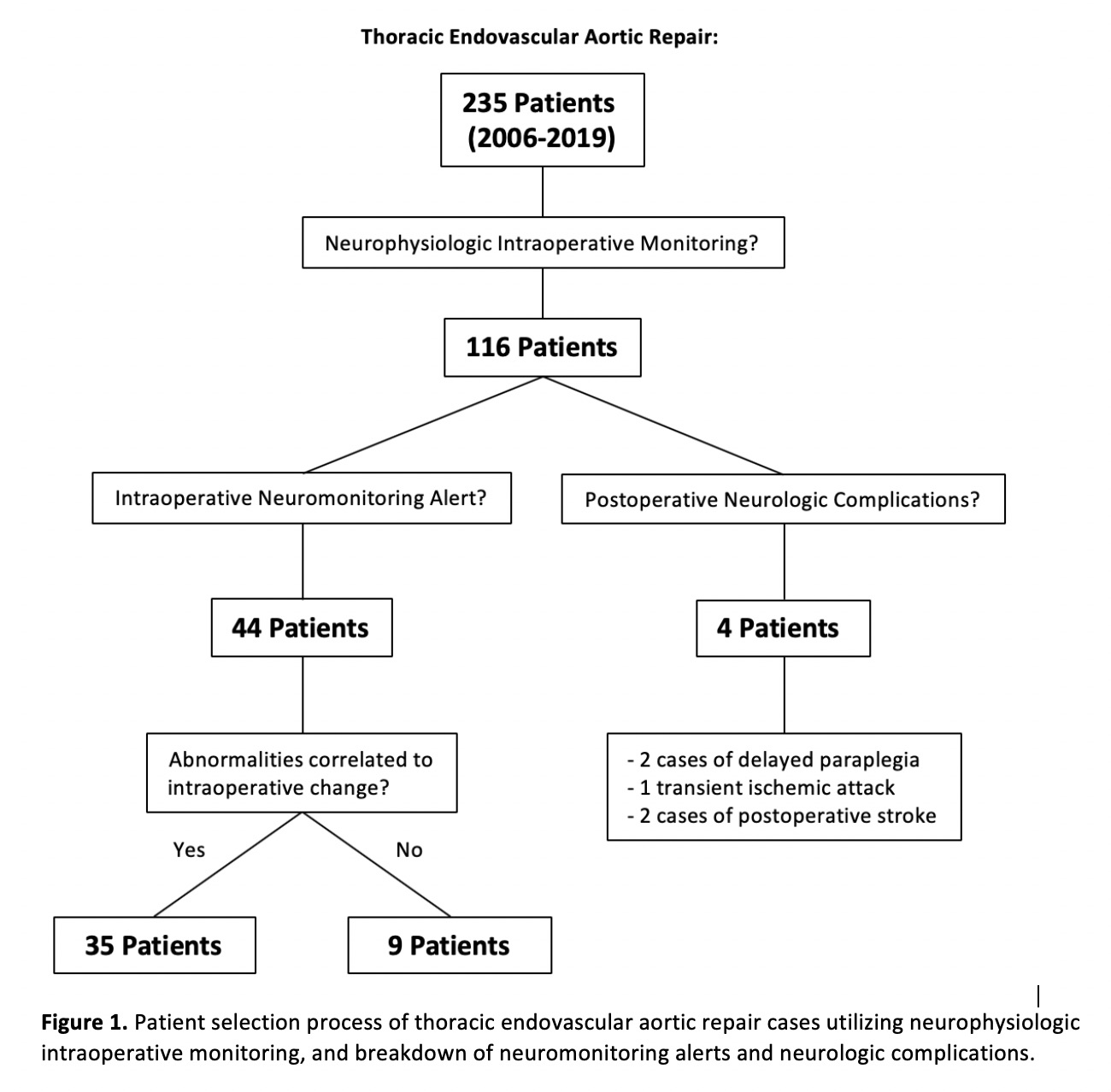
Back to 2020 Posters
