Associations of Regional Prevalence of Peripheral Arterial Disease and Diabetes and Amputation rates Among Medicare Patients
Mark A Eid1, Jonathan A Barnes1, Zachary J Wanken1, Richard J Powell1, David H Stone1, Bjoern D Suckow1, Barbara Gladders2, Mark Creager3, Shipra Arya4, Philip P Goodney1
1Dartmouth Hitchcock Medical Center, Department of Vascular Surgery, Lebanon, NH;2The Dartmouth Institute for Health Policy and Clinical Practice, Lebanon, NH;3Dartmouth Hitchcock Medical Center, Department of Cardiology, Lebanon, NH;4Stanford University School of Medicine, Department of Vascular Surgery, Redwood City, CA
Associations of Regional Prevalence of Peripheral Arterial Disease and Diabetes and Amputation rates Among Medicare Patients
Background:
Prior research has examined associations between the prevalence of peripheral arterial disease (PAD) and amputation risk, especially among high risk populations. However, the effect of concomitant PAD and diabetes on associations with amputation risk has not been explored as extensively, especially in recent patient cohorts.
Methods:
Using data from the Centers for Medicare and Medicaid Services from 2003-2016, we identified a cohort of patients concurrently diagnosed with both PAD and diabetes (N= 10,506,254). Patients were followed from time of diagnosis to identify major and minor amputation events. We examined associations between the regional prevalence of PAD and diabetes and amputation rates, at the level of the state and the hospital referral region (HRR).
Results:
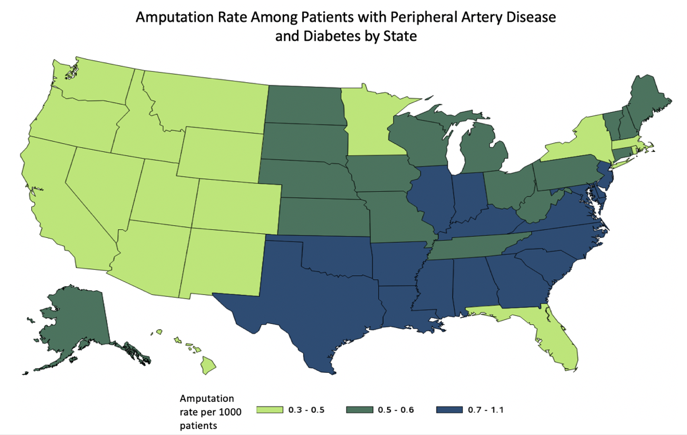
The prevalence of PAD and diabetes across the entire cohort was 15.3 per 1000 Medicare patients, that ranged from 6.7 in Oregon to 27.03 in New Jersey. The average rate of amputation between 2003 and 2016 was 0.6 amputations per 1000 Medicare patients. This rate varied more than 3-fold across states, with rates as low as 0.3 per 1000 Medicare patients in Colorado vs rates of 1.09 per 1000 in Mississippi (Figure 1). States with the highest quartile of amputation risk (0.7 per 1000) were generally clustered in the Deep South (Figure 2). We found a direct and significant association between regional prevalence of PAD and diabetes and amputation risk, at both the state (R2=0.52, P<0.001) and HRR level (R2=.41 P<0.001).
Conclusion:
Regional prevalence of concomitant PAD and diabetes is closely related to amputation risk, and may serve as a more effective guide than PAD alone in identifying patients and regions most likely to benefit from interventions intended to limit amputation. 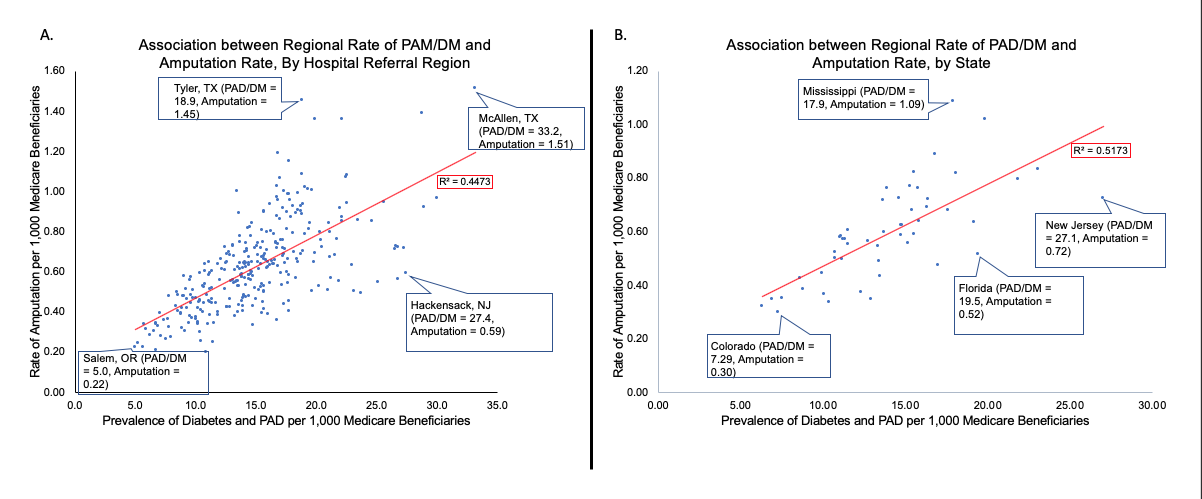
Back to 2020 Posters
