Safety and Efficacy of an Endovascular-First Approach to Acute Limb Ischemia (ALI)
Olia Poursina, Hector Elizondo, Miguel Montero-Baker, Zachary S Pallister, Joseph L Mills, Sr., Jayer Chung
Baylor College of Medicine, Houston, TX
INTRODUCTION: The optimal technique to manage acute limb ischemia (ALI) remains unclear. Prior reports suggest that the decreased morbidity and mortality of endovascular approaches are mitigated by limited technical success rates relative to open or hybrid approaches for ALI. These data failed to include newer technologies that may improve technical success rates. We therefore sought to describe current outcomes of an endovascular-first approach to ALI.
METHODS: Single-center, single-arm, retrospective review of consecutive patients presenting with ALI from 2015-2018. All patients underwent an endovascular-first approach. Technical success, limb salvage, survival, patency, and hospital length of stay were quantified with Kaplan-Meier analyses. Cox regressions were used to identify predictors of amputation-free survival.
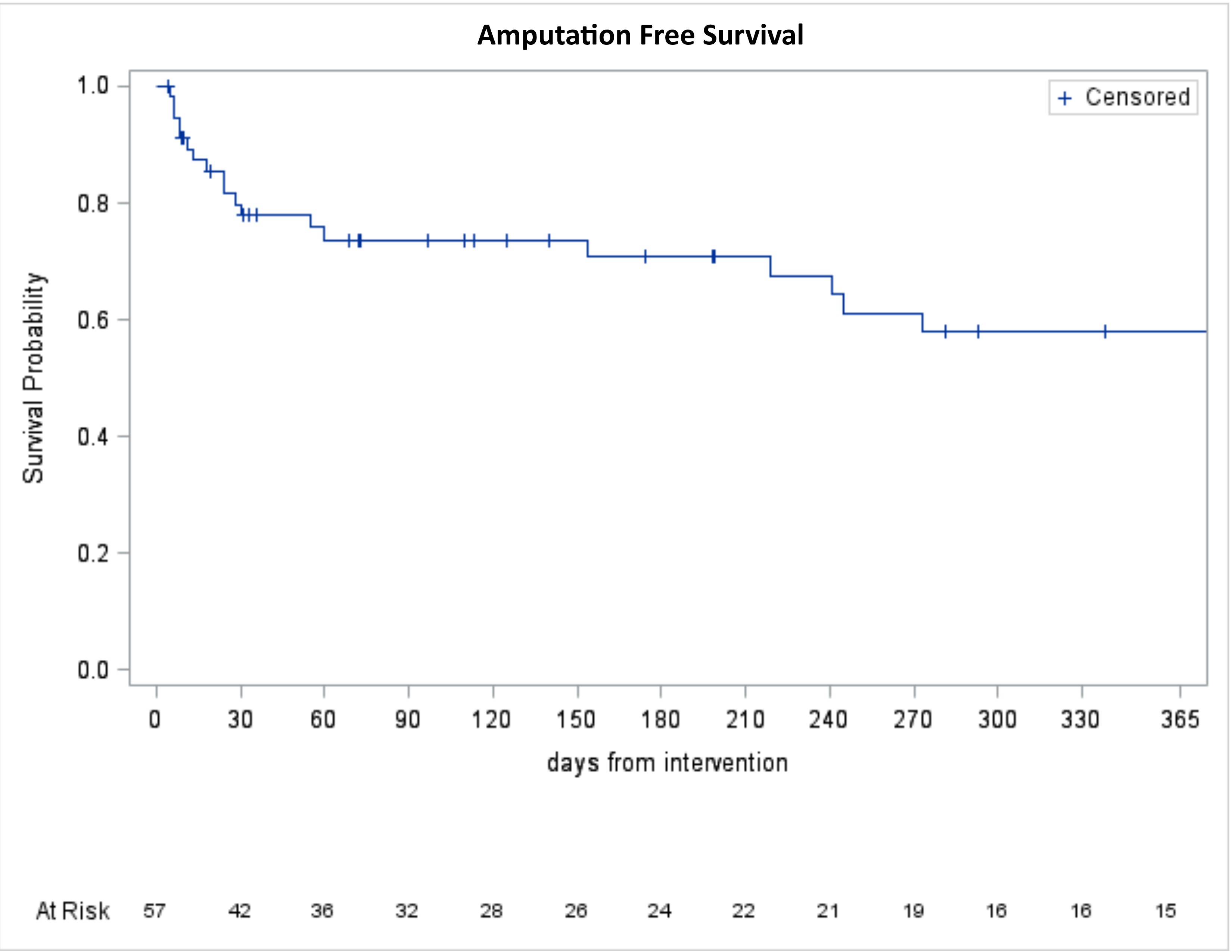
RESULTS: Over three years, 60 patients (39 = male; 65%) with 60 symptomatic limbs presented with ALI (Rutherford Class: I=15 (25%); IIa=23 (38%); IIb=13 (22%); and III=9 (15%). The median age was 65 years (IQR 59, 75). A history of prior failed ipsilateral revascularization was present in 34 (57%; 8 (13%) open bypass; 8 (13%) endovascular; 18 (30%) both open and endovascular). There were 19 (32%) patients who underwent catheter-directed thrombolysis (CDT) only, while 19 (32%) underwent CDT in combination of aspiration and/or rheolytic thrombectomy. 16 patients (27%) underwent only aspiration and/or rheolytic thrombectomy. The remainder underwent primary covered stent placement without thrombolytics, or percutaneous thrombectomy. Adjunctive endovascular procedures were performed in 53 (88%), consisting of 25 (42%) balloon angioplasty and stent placements; 22 (37%) balloon angioplasties only; and 6 (10%) atherectomies with/without angioplasty and stenting. Technical success was achieved in 58 (97%), and required open conversion in 2 (3%), which consisted of one common femoral endarterectomy and one graft embolectomy. At thirty days, 52 (87%) survived, and 53 (88%) with successful limb salvage. Five patients (8%) underwent four-compartment fasciotomy. Other complications included myocardial infarction/arrhythmia in 7 (12%), acute kidney injury in 10 (17%). There were no major hemorrhagic complications. Median length of stay overall and in the intensive care unit were 9 (IQR 4, 14) days and 2 (IQR 1, 5) days, respectively. At one year, Kaplan-Meier estimates for the following were: amputation-free survival 58% + 4.2% (Figure 1); survival 73% + 2.7%; limb salvage 75% + 2.6%. Multivariable analysis revealed that only a history of prior myocardial infarction independently predicted death/major amputation (HR=2.5, 95% CI 1.03-6.1; p = 0.04; Table 1).
CONCLUSIONS:Contrary to prior reports, current endovascular approaches to ALI have high technical success rates. With an endovascular-first approach to ALI, survival and limb salvage are similar to historical open surgical outcomes, while fasciotomy rates, perioperative complications, and length of stay are lower. Further prospective evaluation with appropriately powered multi-center cohorts is warranted to evaluate the efficacy of endovascular versus open approaches to ALI.
| Variable | Unadjusted HR (95% CI) | p | Adjusted HR (95% CI) | p |
| History of myocardial infarction | 2.5 (1.03-6.1) | 0.04 | 2.5 (1.03-6.1) | 0.04 |
| History of hypercoagulable disorder | 2.4 (0.83-6.7) | 0.11 | ||
| Rutherford Class | 1.3 (0.96-1.8) | 0.09 |
Back to 2020 Posters
