Autologous Femoral Vein is a Viable Conduit for Femoral-femoral Artery Bypass: A Single Institution Experience
Nicholas Lysak, Thomas Huber, Salvatore Scali, Javairiah Fatima
University of Florida, Gainesville, FL
Introduction: Infections of vascular grafts involving femoral artery carry significant morbidity and mortality, often requiring complex vascular reconstructions for remediation in an infected field which limits choice of conduits. Herein we describe our institution’s experience with femoral-femoral artery bypass using autologous femoral vein.
Methods: All patients who underwent femoral-femoral artery bypass using autologous femoral vein conduit between 2003 and 2018 were included in this study. Demographic, operative, and outcomes data was extracted from the EMR. Primary end-points were in-hospital and 1-year mortality, secondary end-points included survival, graft reinfection, and reintervention.
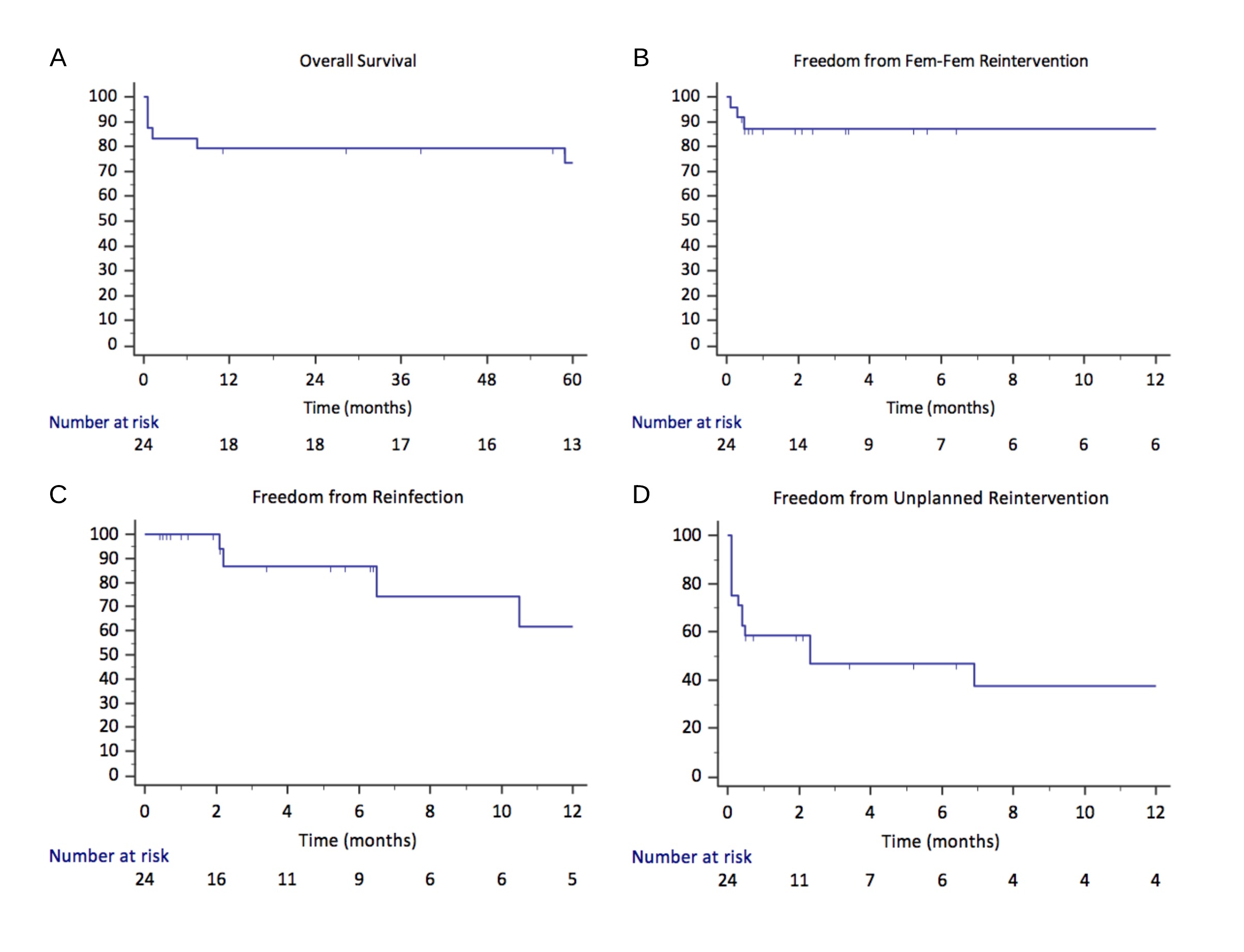
Results: Twenty-three patients (12 males, age 59±3 years) underwent 24 femoral-femoral artery bypass procedures using autologous femoral vein conduit. Twenty-one (86%) patients underwent this procedure for prior graft infections. Median time from initial graft placement to presentation with infection was 14 months (range 0-250 months). Fourteen (58%) patients underwent isolated femoral-femoral bypass, 7 (29%) underwent simultaneous aortic inflow procedure, and 3 (13%) underwent simultaneous outflow procedure. Most common presentation was abscess formation in 14 (58%) and cellulitis in 12 (50%) patients. Cultures were positive in 50% with most common organism being Staphylococcus aureus. In-hospital and 1-year all-cause mortality was 13% and 21% respectively. Major complications occurred in 13 (54%) patients (Table1). Overall graft reintervention rate was 13%. No patient developed subsequent infection of the femoral-femoral vein graft, though 4 (19%) developed recurrent infections of remainder of prosthetic bypass material. Two (8%) patients required amputation and both died within 1 year. Composite major adverse limb event (MALE) rate was 17%. Median follow-up was 5 months (range 0-129 months). Overall one-year and 5-year survival were 83±8% and 74±9% respectively, freedom from femoral-femoral bypass reintervention was 87±7% at 1 year, freedom from any unplanned reintervention at 6 months and 1 year were 47±10% and 37±12% respectively, and freedom from recurrent infection of remaining graft material at 6 months and 1 year were 87±7% and 65±13%, respectively (Fig. 1).
Conclusions: Autologous femoral vein is a viable choice for femoral-femoral artery bypass, in the setting of limited conduit options in grossly infected field, with low reintervention and reinfection rates, and acceptable outcomes.
Table 1. Outcomes
| All Cohort | |
| In-hospital mortality, n (%) | 3 (13) |
| 1-year mortality, n (%) | 5 (21) |
| Unplanned re-operation, n (%) | 9 (38) |
| Re-operation on femoral-femoral bypass, n (%) | 2 (8) |
| Re-operation indication, n (%) | |
| Femoral-femoral bypass occlusion | 1 (8) |
| Other thrombus | 3 (23) |
| Bleeding | 2 (15) |
| Compartment Syndrome | 2 (15) |
| Infection/Abscess | 2 (15) |
| Other | 4 (17) |
| Time to reoperation, median days (IQR) | 3 (1 – 11.5) |
| Complications, n (%) | |
| Femoral-femoral graft occlusion | 1 (4) |
| Other thrombus | 3 (13) |
| Compartment syndrome | 2 (8) |
| Amputation | 1 (4) |
| Bleeding/Hematoma | 3 (13) |
| Pneumonia | 3 (13) |
| Acute kidney injury | 2 (8) |
| GI bleed | 1 (4) |
| Wound infection | 1 (4) |
| Venous thromboembolism | 1 (4) |
| After discharge | |
| Infection of remaining prosthetic graft, n (%) | 4 (19) |
| Subsequent operation, n (%) | 11 (52) |
| Re-intervention on femoral-femoral bypass, n (%) | 1 (5) |
| Amputation, n (%) | 1 (5) |
IQR, Interquartile Range
Back to 2020 Posters
