Single-center experience with the femoral-to-brachial preloaded delivery system for fenestrated-branched endovascular repair of complex aortic aneurysms
Guilherme BB. Lima1, Aleem K Mirza1, Emanuel R Tenorio1, Giulianna B Marcondes1, Marina Dias-Neto1, Naveed Saqib1, Bernardo C Mendes2, Gustavo S Oderich1
1The University of Texas Health Science Center at Houston, Houston, TX;2Division of Vascular and Endovascular Surgery Mayo Clinic, Rochester, MN
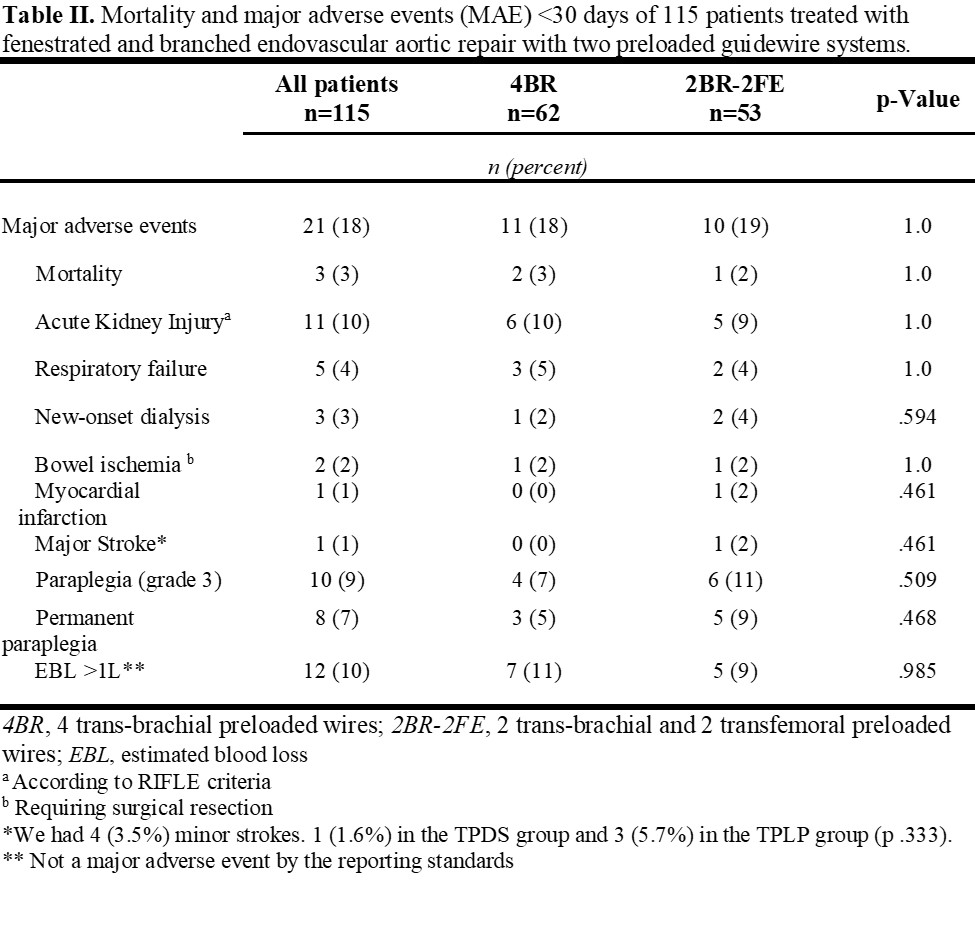
Background: The role of fenestrated-branched endovascular aortic repair (FB-EVAR) in the treatment of complex aortic pathology has evolved rapidly over the last two decades. Much of this is due to the development and selective use of procedural adjuncts, such as low-profile devices, upper extremity (UE) access, and preloaded delivery systems (PDS). Our experience with femoral-to-brachial (FTB ) preloaded delivery system (PDS) has advanced over the years. The aim of this study was to assess technical aspects and outcomes of FB-EVAR using FTB-PDS with two separate configurations. Methods: Clinical data of 430 consecutive patients enrolled in a prospective non-randomized study to evaluate FB-EVAR for pararenal (PRA) and thoracoabdominal aortic aneurysms (TAAA) between 2013 and 2020 was reviewed. Patients treated with FTB-PDS were included. The two configurations included 4 trans-brachial preloaded wires (4BR) or 2 trans-brachial and 2 transfemoral preloaded wires (2BR-2FE). Endpoints included technical success, procedural metrics (fluoroscopy time, radiation dose, contrast volume, operative time), 30-day or in-hospital mortality, major adverse events (MAEs), and target-vessel outcomes. Results: There were 115 patients, 65% male and 25% female with a mean age of 73.8±8 years, treated with FTB-PDS. Of these, 62 patients (54%) had 4BR and 53 patients (46%) had 2BR-2FE FTB-PDS, with similar cardiovascular risk factors and aneurysm extent. There were 106 TAAA (92%) and 9 PRA (8%) with a mean of 3.9±0.5 targeted vessels per patient. Fenestrations were less commonly used in the 4BR group (54% vs. 77%, P<.001). Technical success was 97%, with no differences in total operating time (236 vs. 242 minutes, P=.78), endovascular time (154 vs. 165 minutes, P=.77), radiation dose (1.1 vs.1.2 Gy, P=.79), and contrast volume (151 vs. 140 mL, P=.52) between the 4BR and 2BR-2FE groups, respectively (Table I). There were 3 deaths (3%) at 30 days or during the hospital stay. MAEs were noticed in 21 patients (18%) with no difference between groups (18% vs. 19%, P=1.0), including new-onset dialysis (2% vs 4%, P=.59), and paraplegia (7% vs 11%, P=.51), for 4BR and 2BR-2FE, respectively (Table II). After a mean follow-up of 15±11 months, patient survival and freedom from aortic-related mortality at 2-years were 78.8±5% and 96.5±1.7% respectively, with no difference between groups. Target artery primary patency and freedom from target artery instability were 93±2.2% and 89.2±2.5%, respectively at 2 years, with also no differences between groups. Conclusion: The use of FTB-PDS for FB-EVAR is safe with high technical success and a low rate of MAEs. Each configuration provides specific benefits based on patient anatomy while having similar procedural metrics and clinical outcomes. 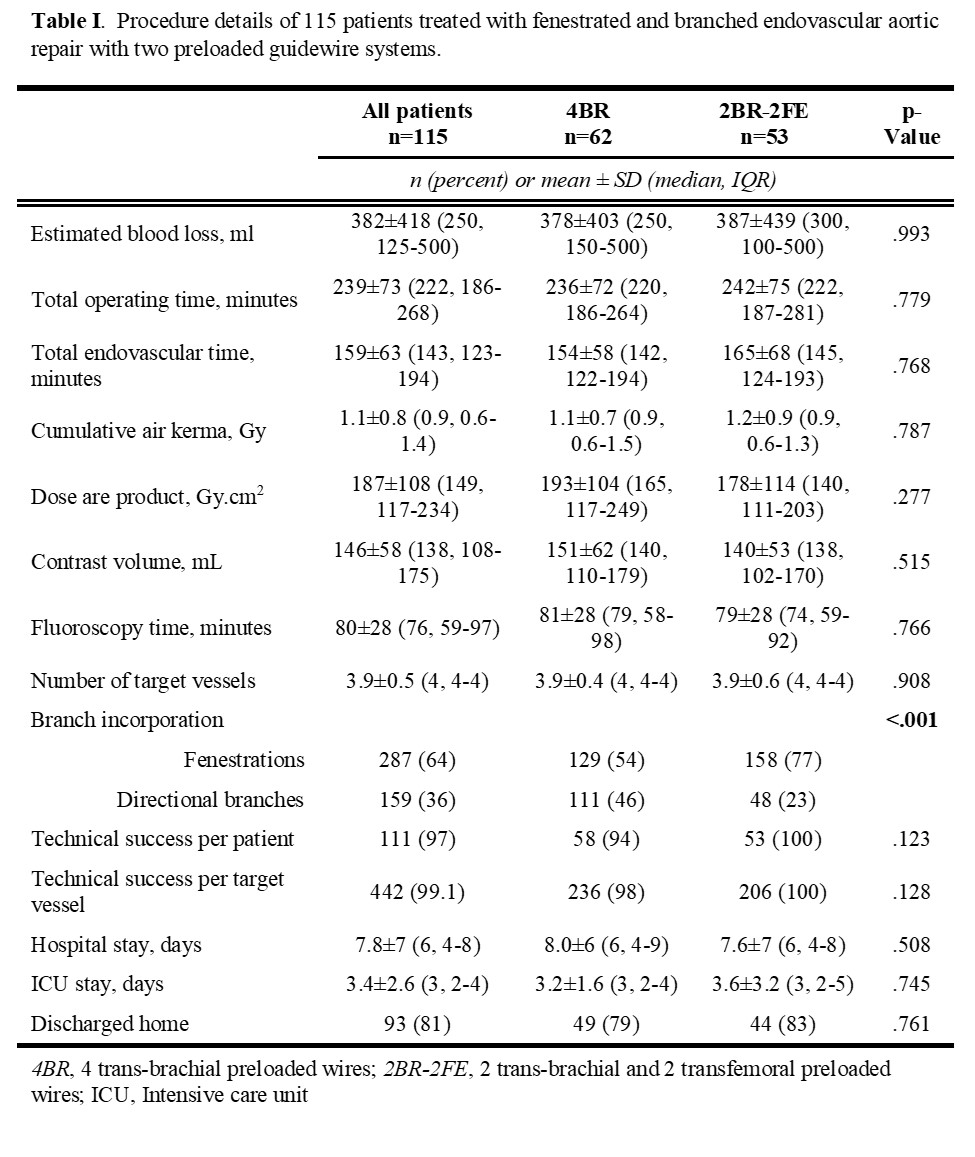
Back to 2022 Abstracts
