Effect of Timing of TEVAR after Type B Aortic Dissection in the SVS VQI Post approval Project for Dissection
Adam W Beck1, Grace Wang2, Joseph Lombardi3, Rodney White4, Jack Cronenwett5, John Kern6, Richard P Cambria7, Ali Azizzadeh8
1University of Alabama at Birmingham, Birmingham, AL;2Hospital of the University of Pennsylvania, Philadelphia, PA;33- Division of Vascular and Endovascular Surgery, Cooper University Hospital, Camden, NJ;44- Vascular Surgery Services, Long Beach Memorial Heart & Vascular,, Long Beach, CA;5Dartmouth-Hitchcock Medical Center, Lebanon, NH;66- Division of Thoracic and Cardiovascular Surgery, University of Virginia, Charlottesville, VA;7St. Elizabeth's Medical Center, Brighton, MA;8Cedars-Sinai Medical Center, Los Angeles, CA
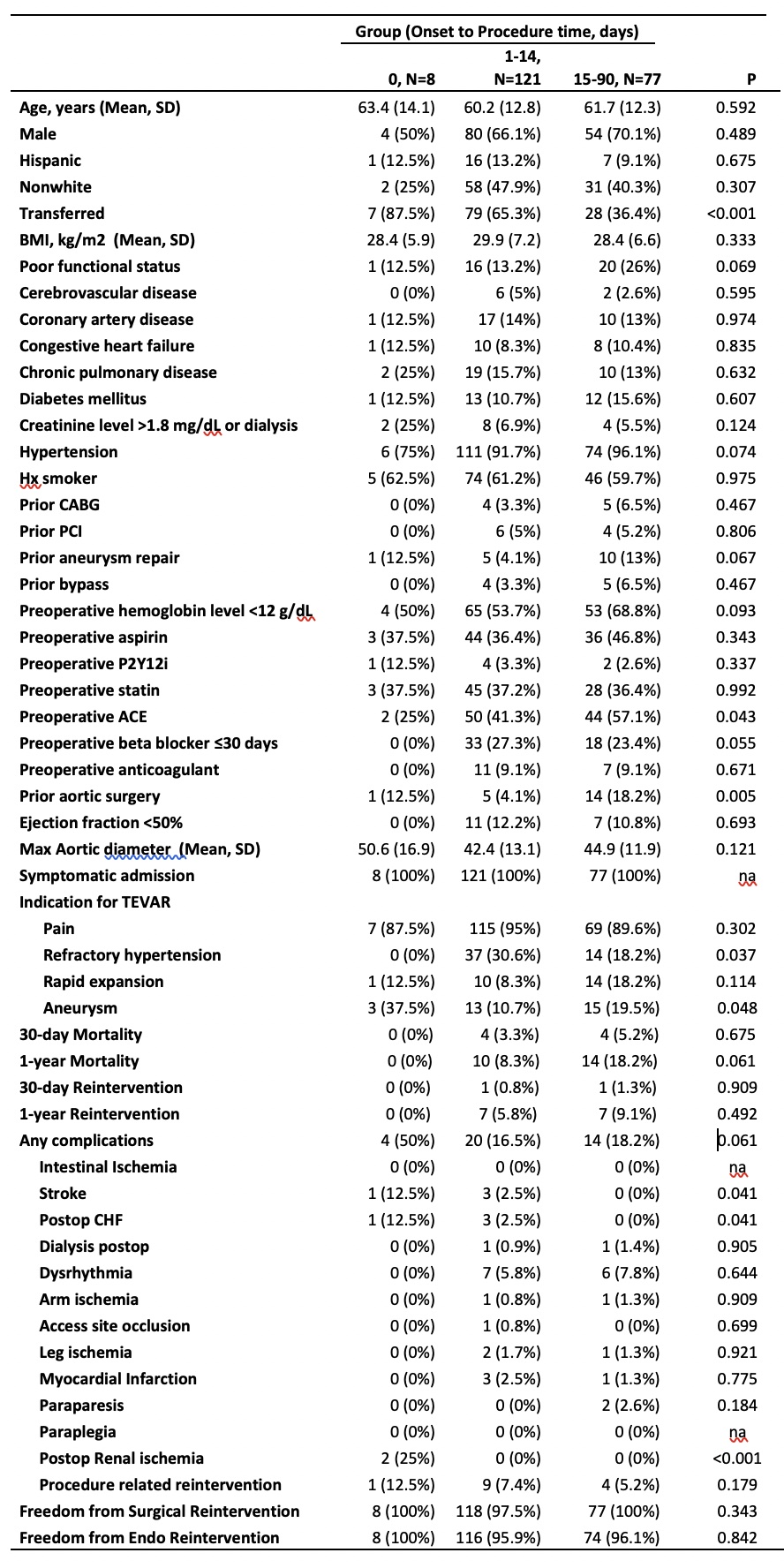
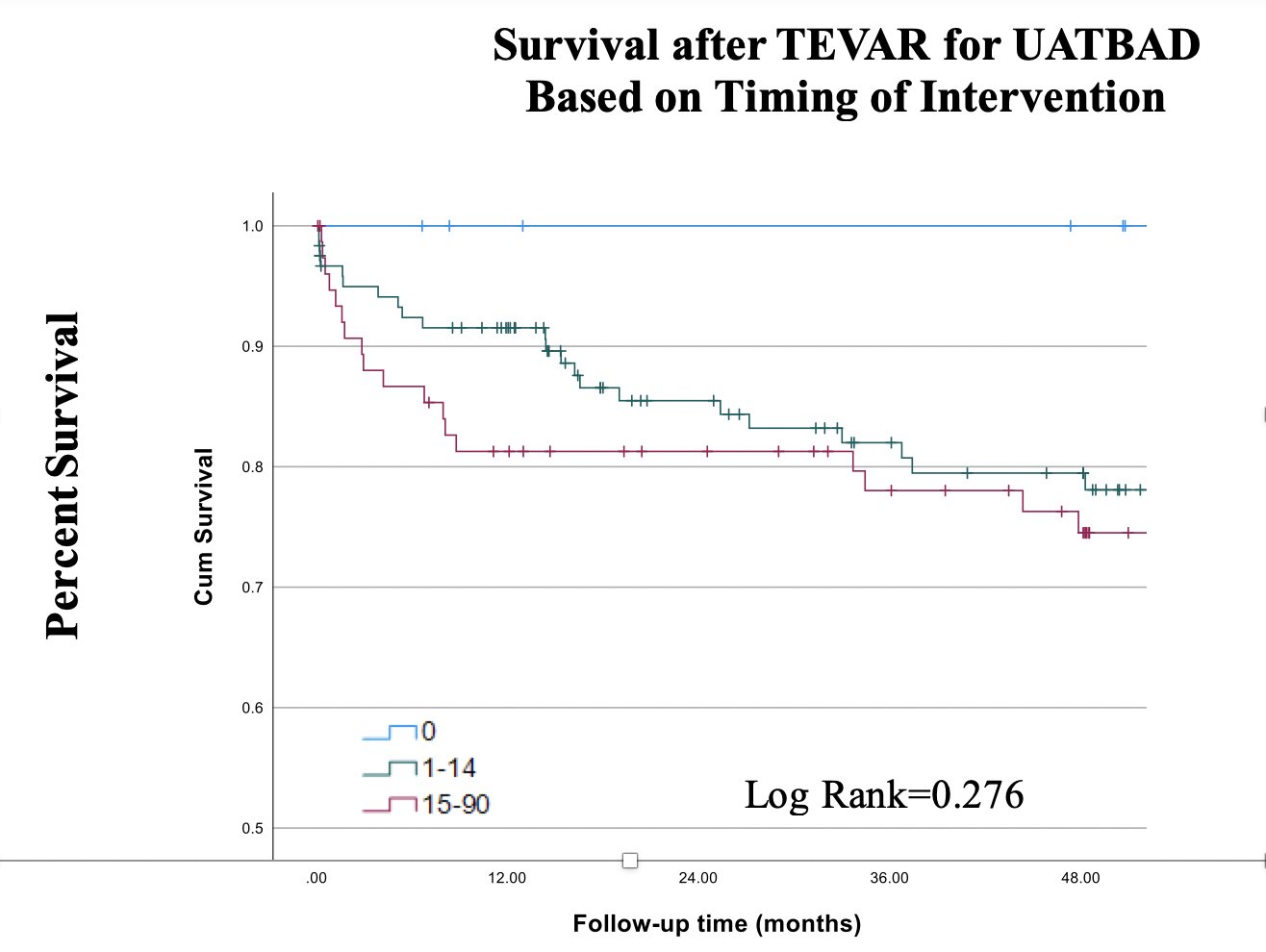
Objective: The timing of TEVAR after the onset of uncomplicated acute type B aortic dissection (UATBAD) remains controversial. The objective of this study was to evaluate the SVS VQI post-approval study (VQI PAS) data for the impact of TEVAR timing for UATBAD on early and late outcomes, including mortality, procedural complications and long-term reintervention. Methods: The VQI PAS includes a total of 606 patients. Patients with UATBAD (defined as those without rupture or malperfusion) exclusive of cases categorized as emergent (N=206), were divided into groups defined by the SVS/STS reporting guidelines based on timing of treatment after the onset of dissection. Groupings were: within 24 hours (N=8), 1-14 days (N=121), and 15-90 days (N=77). Univariate and multivariable analysis was used to determine differences between timing groups for postoperative mortality, in-hospital complications, and reintervention. Results: Patients were very similar across the 3 TEVAR timing groups based on demographics and comorbid conditions. Notable differences included a higher prevalence of baseline elevated creatinine (>1.8mg/dL)/chronic ESRD and designation as “urgent” in the <24-hour group, as well as a higher rate of pre-operative beta-blocker therapy in the 1-14 day group (table). Unadjusted 30-day mortality across groups was not different (0%, 3.3%, 5.2% P=0.68), nor was 1-year mortality (0%, 8.3%, 18.2%; P=0.06). Post-operative stroke, CHF, and renal ischemia were more common in the <24-hour group (table). Reintervention out to three years was not different between the groups. Multivariable analysis demonstrated presence of postoperative therapeutic lumbar drain to be the only a predictive risk factor for mortality (HR 8.96, P=0.004). Conclusions: There appears to be a survival benefit of intervention in the 1-14 day period of UATBAD in this real world dataset. This benefit was without an increase in post-operative complications compared to patients treated 15+ days after dissection and with a trend towards lower mortality for the 1-14 day group. Consistent with previous studies, patients treated in the hyperacute (<24 hour) phase are higher risk and had higher postoperative complications.
Back to 2022 Abstracts
