Contemporary Management of Acute Type B Intramural Hematoma in the Endovascular Era
Charles Crepy D'Orleans, Yazan M. Duwayri, Alysa B. Zellner, Woodrow J. Farrington, W. Brent Keeling, William D. Jordan, Jr., Bradley G. Leshnower
Emory University School of Medicine, Atlanta, GA
INTRODUCTION: Acute type B intramural hematoma(ATBIMH) is typically considered a more benign pathology than aortic dissection. Historically, ATBIMH was managed with optimal medical therapy(OMT) and in-hospital mortality rates were comparable to acute type B aortic dissection. The purpose of this study is to evaluate contemporary outcomes of the management of ATBIMH in the endovascular era.
METHODS: A retrospective analysis of a U.S. academic aortic database identified 71 patients diagnosed with ATBIMH between 2008 and 2020. Patient records were reviewed and contrast cross-sectional imaging exams were analyzed using aortic centerline techniques. All patients were initially managed with optimal medical therapy(OMT) including anti-impulse therapy. Patients were grouped based on first line management: early thoracic endovascular aortic repair(TEVAR;Group 1) or hospital discharge on OMT(Group 2). Patients in the Group 2 were sub-categorized into delayed surgical intervention(Group 2-A) or no surgical intervention(Group 2-B). Retrograde type A dissection or IMH were excluded.
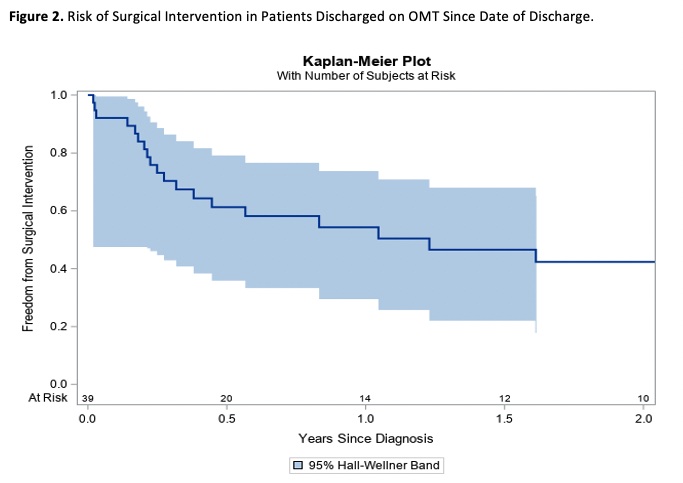
RESULTS: Of 71 total patients, 45% patients(n=32) underwent TEVAR(Group 1) and 55% (n=39) were discharged on OMT(Group 2)(Figure 1). There were no significant differences in age, demographics, or medical comorbidities between the two groups. In Group 1, 28 patients(39%) underwent emergent TEVAR due to the presence of a penetrating aortic ulcer(PAU) or ulcer-like projection(ULP)(n=25), aortic aneurysm(n=2), or type B aortic dissection(n=1). Operative mortality was 3%(n=1). No patient suffered a stroke or spinal cord ischemia. Radiographically, patients in Group 1 had larger maximum aortic diameters(53±15mm vs. 45±12mm, p=0.005), longer IMH extents longitudinally(292±100mm vs. 229±98mm, p=0.01), and were more likely to present with PAUs(92% vs. 55%, p=0.003) and ULPs(57% vs. 10%, p=0.01). During the follow-up period, 49%(n=19) patients required delayed surgical intervention(Group 2A), including TEVAR in 16 patients and open aortic repair in 3 patients(Figure 2). 20 patients did not require any surgical intervention(Group 2B). There were no differences in age, demographics, or comorbidities between Groups 2A and 2B. The indications for surgical intervention in Group 2A included the development or progression of a PAU or ULP(n=11), progression to type B dissection(n=4), thoracic aortic aneurysm(n=3), and IMH expansion(n=1). Radiographically, only the presence of PAUs was significantly greater in Group 2A (79% vs. 33%, p=0.01). Of the initial cohort ATBIMH, 72%(n=51) of patients required surgery, including 68%(n=48) who were successfully treated with TEVAR.
CONCLUSIONS: ATBIMH treated with OMT has a high incidence of failure. A contemporary treatment algorithm with endovascular therapy can be accomplished with low perioperative morbidity and mortality and results in excellent overall survival. At the index hospitalization, ATBIMH with a source lesion should undergo TEVAR. Patients discharged on OMT require close radiographic surveillance as there is an elevated risk of developing focal aortic pathology that is optimally treated with short segment TEVAR. 
Back to 2023 Posters


