Factors Impacting Reintervention for Patients Who Underwent Infrainguinal Revascularization at a Single Hospital System, 2016-2019
Dominique M Dockery1, Krissia Rivera Perla1, Joao Filipe G Monteiro2, Robert B Patterson1, Carla C Moreira2
1Alpert Medical School of Brown University, Providence, RI;2Rhode Island Hospital, Providence, RI
Background: A limited number of studies have examined the impact of social determinants of health on peripheral arterial disease (PAD) but there are few studies that follow individual patients through re-interventions. We compared patients who underwent infrainguinal revascularization (endovascular, open, or hybrid) requiring any reintervention (AR) within the first year to those who did not (NR), to identify risk factors and analyze differences in outcomes.
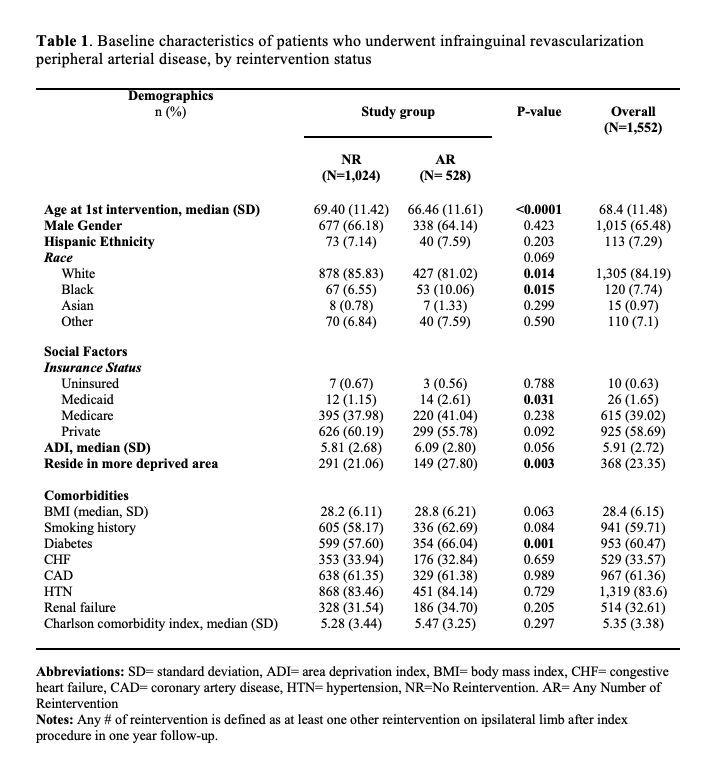
Methods: A retrospective study identified 1,552 index procedures between 2016-2019, demographics, comorbidities, re-interventions, and outcomes for the index-extremity were identified within 1-year follow-up period. Multivariate logistic regression analysis was conducted in SAS software to compare the two study groups. The model was controlled for age, race, smoking history, insurance status, residence in more deprived areas, diabetes, Charlson comorbidity index, and 1-year complications.
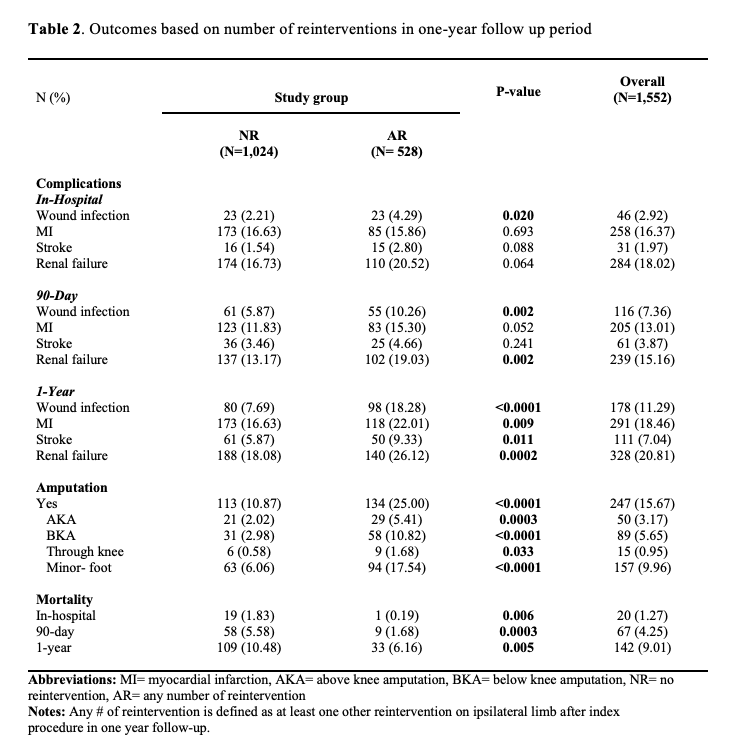
Results: Thirty-four percent of the patients had reintervention. Reintervention patients were on average younger (66.5-years, 69.4-years [NR], p-value=<0.001), Black race (10.1%, 6.6% [NR], p-value=0.015), diabetic (66.0%, 57.6% [NR], p-value=0.0010), have Medicaid insurance (2.6%, 1.2% [NR], p-value=0.0315), and residing in more deprived areas (27.8%, 21.1% [NR], p-value=0.0038). Following any reintervention, patients had higher rates of amputations (25%, 10.9% [NR], p-value=<0.0001) and wound infections (18.28%, 7.69% [NR], p-value=<0.0001), but reduced mortality at one-year (6.16%, 10.48% [NR], p-value=0.005). In multivariable analysis, risk factors associated with reintervention included residence in more deprived areas (OR 1.29 with 95% CI [1.00-1.67]), age less than 67 years (1.39 [1.11-1.74]), Medicaid insurance (2.24 [1.01-4.97], history of diabetes (1.38 [1.05-1.81], smoking (1.41 [1.12-1.77]) and wound infection (2.27 [1.61-3.19]).
Conclusion: Undergoing any reintervention following index-lower extremity revascularization is associated with higher rates of amputation and complications at one-year. Risk factors associated with reintervention include younger age, living in more deprived areas, Medicaid insurance, history of diabetes mellitus, smoking, and post-operative wound infections. Additional research is needed to identify modifiable risk factors for reintervention in PAD care.
Back to 2023 Posters


