Predictors of Rapid Failure of Medical Management in Uncomplicated Acute Type B Aortic Dissection
Elizabeth L Norton, Yuqing Wang, Jose N Binongo, Yazan M Duwayri, Edward P Chen, William D Jordan, Jr., Bradley G Leshnower
Emory University, Atlanta, GA
INTRODUCTION: The optimal management strategy for acute uncomplicated type B aortic dissections(auTBAD) remains undetermined. Optimal medical therapy(OMT) provides excellent short-term outcomes but is associated with a high incidence of failure in the chronic phase. This study sought to identify risk factors for rapid failure of OMT in auTBAD.
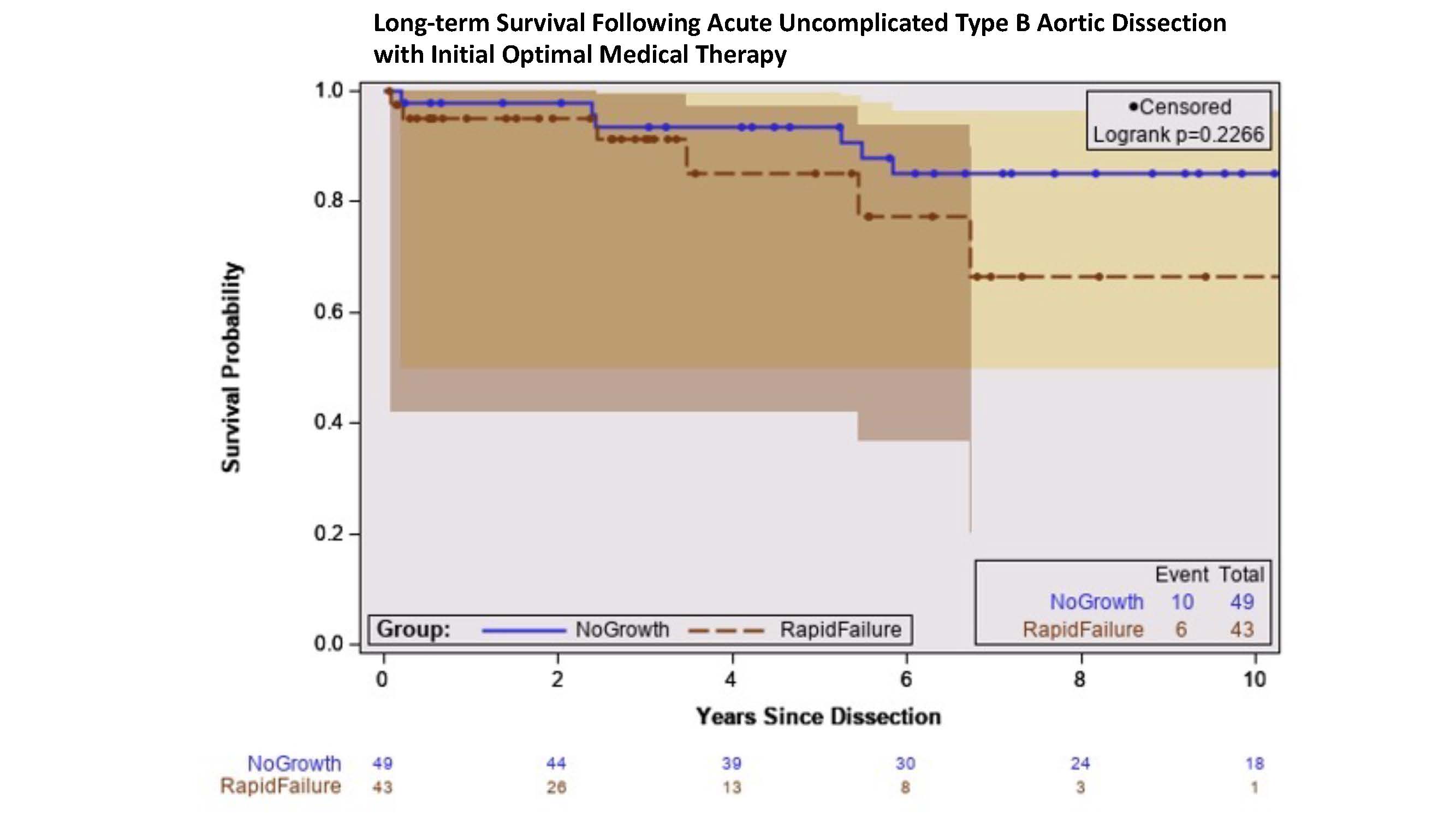
METHODS: A retrospective analysis of a U.S. aortic database identified 410 patients from 2000-2022 who were diagnosed with auTBAD and underwent initial management with OMT. From this cohort, 92 patients with ≥2 contrast-enhanced imaging scans were divided into two groups: (1)NG-OMT(No Growth): 49 patients with no growth (defined as <10mm) who were managed with definitive medical therapy and (2)RF-OMT(Rapid Failure): 43 patients who underwent open or endovascular surgery due to OMT failure within 3 years of their dissection due to rapid growth and/or aneurysmal degeneration. Patient demographics and contrast imaging exams were analyzed from the time of dissection. Multivariable logistic modelling determined risk factors for rapid OMT failure and Kaplan-Meier estimate was used to compute long-term survival.
RESULTS: The mean age was 52 years and was similar between groups(NG-OMT 52 vs RF-OMT 56 years, p=0.13). The RF-OMT group had more males(72% vs 51%, p=0.04), less smoking history(30% vs 45%, p=0.02), and less chronic kidney disease(7% vs 22%, p=0.04). The RF-OMT group more frequently had a Zone 3 primary intimal tear(PIT) (43% vs 12%, p<0.001) and had a greater number of thoracic intimal tears in the RF-OMT group (1.6 vs 1.1, p=0.01) compared to the NG-OMG group. The average time from diagnosis of auTBAD to surgical intervention in the RF-OMT group was 8.4 months. At time of surgery in RF-OMT patients, the descending thoracic aortic diameter had increased from 44 mm(IQR25-75%: 41,56) at the time of dissection to 59 mm(IQR25-75%: 52, 66). Surgical intervention included thoracic endovascular aortic replacement(45%), arch replacement with frozen elephant trunk(10%), open descending thoracic aortic replacement(29%), and thoracoabdominal aortic replacement(17%). Thirty-day mortality among the RF-OMT patients was 4.7%. Smoking history (OR=4.38, 95% CI: [1.43, 13.36], p=0.01], PIT in Zone 3 (OR=15.56, 95% CI:[3.80, 63.65], p=0<0.001), and thoracic aortic diameter (OR=2.05, 95% CI: [1.41, 3.32], p=0<0.001) were independent risk factors for rapid OMT failure in auTBAD(Table). Long-term survival from date of dissection was worse in the RF-OMT group at 8 years (RF-OMT 66% vs NG-OMT 85%, p=0.23)(Figure).
CONCLUSIONS: Patients with an auTBAD, who have a smoking history, a Zone 3 PIT, and an aneurysmal descending thoracic aorta >43 mm should be considered for TEVAR in the acute phase due to the high risk of rapid OMT failure.
| Odds Ratio [95% Confidence Interval] | p-value | |
| Smoking history | 4.38 [1.443, 13.36] | 0.01 |
| PIT in Zone 3 (vs Zone 4) | 15.56 [3.80, 63.65] | <0.001 |
| PIT in Zone 3 (vs Zone 5) | 12.85 [2.75, 59.97] | 0.001 |
| Descending thoracic aortic diameter | 2.05 [1.41, 3.32] | <0.001 |
Back to 2023 Posters


