Open Bypass Is Superior To Endovascular Revascularization In Patients Undergoing Reintervention For Chronic Limb Threatening Ischemia Using a Medicare-Linked Database
Nadin S Elsayed1, Marc L Schermerhorn2, Mahmoud B Malas1
1University of California San Diego, San Diego, CA;2Beth Israel Deaconess Medical Center, Boston, MA
INTRODUCTION: The need for re-interventions following lower extremity revascularization(LER) is common, ranging from 13% and up to 85% depending on different follow-up periods. Prior literature has detailed the outcomes of bypass therapy(BT) and endovascular therapy(ET) in patients undergoing initial LER for chronic limb-threatening ischemia(CLTI). Nonetheless, there is a paucity of data regarding the best revascularization technique for patients undergoing re-intervention following prior revascularization. This study aims to describe the outcomes of BT versus ET in patients with prior open or endovascular LER to determine the best modality of revascularization in this large patient population.
METHODS: We identified all patients with a history of prior ipsilateral LER who had undergone LER from 2010 to 2019 in the VQI-VISION database. Patients who had undergone suprainguinal procedures were excluded. Study groups included: BT versus ET in patients with prior ET and BT versus ET in patients with prior BT. Outcomes included 1- and 5-year major amputation or death, major amputation, revascularization, and all-cause mortality (ACM). RESULTS: A total of 17,145 patients had undergone prior ET with 69.7% undergoing redo ET and 30.3% undergoing BT, and 15,905 patients had undergone prior BT with 83.7% undergoing ET and 16.3% undergoing redo BT. Among patients with prior ET, Patients undergoing BT were more likely to be males (60.6% vs 58.1%, P=0.002) and smokers (79% vs 67.1%, P<0.001). They were also more likely to present with rest pain (38.8% vs 27%, P<0.001) and lower ankle-brachial index (ABI) (0.6 ± 0.6 vs 0.8 ± 0.6, P<0.001). After adjusting for confounders, BT was associated with lower risk of one-year major amputation or death (aHR: 0.75, 95%CI(0.7-0.8), P<0.001), ACM (aHR: 0.8, 95%CI(0.7-0.9), P<0.001), major amputation (aHR: 0.7, 95%CI(0.6-0.8), P<0.001), and revascularization (aHR: 0.76, 95%CI(0.7-0.9), p<0.001). Among patients with prior BT, redo BT patients were more likely to be males (65.9% vs 58.6%, P<0.001) and smokers (86.2% vs 67.7%, P<0.001). They were also more likely to present with rest pain (46.7% vs 27.8%, P<0.001) and lower ABI (0.5 ± 0.5 vs 0.8 ± 0.6, P<0.001). After adjusting for confounders, redo BT was associated with improved one-year major amputation or death (aHR: 0.8, 95%CI(0.7-0.9), P<0.001), ACM (aHR: 0.7, 95%CI(0.67-0.8), P<0.001), major amputation (aHR: 0.8, 95%CI(0.7-0.9), P=0.008), and revascularization (aHR: 0.76, 95%CI(0.7-0.8), p<0.001). These results persisted for 5 years(Table 1, Figure 1).
CONCLUSIONS: The present study shows that ET is performed more frequently in patients with prior BT or ET. Despite a higher percentage of rest pain and lower ABI in patients undergoing BT, BT had better outcomes with improved limb salvage, durability, AFS, and ACM compared with ET. To date, this is the first and largest real-world analysis showing the superiority of BT over ET in patients with prior BT or ET. 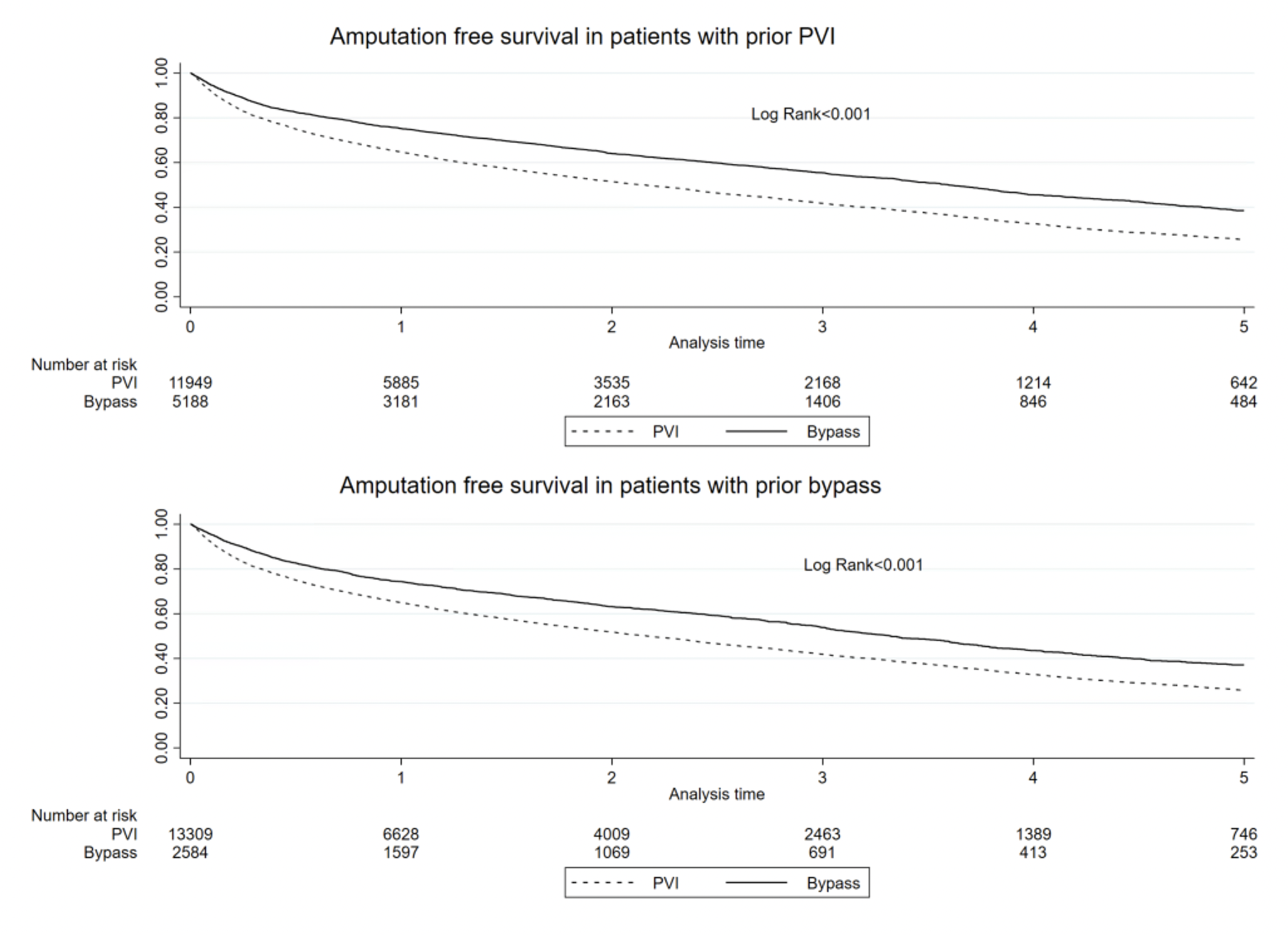
| Prior PVI | Endovascular Therapy (ET)(%) | Bypass Therapy (BT)(%) | Log Rank | Bypass vs PVI HR(95%CI) | P value |
| Amputation or death | 74.3 | 61.5 | <0.001 | 0.77 (0.7-0.8) | <0.001 |
| Mortality | 66.4 | 51.4 | <0.001 | 0.78 (0.7-0.8) | <0.001 |
| Major amputation | 25.2 | 19.2 | <0.001 | 0.7 (0.6-0.8) | <0.001 |
| Revascularization | 63 | 51 | <0.001 | 0.7 (0.7-0.8) | <0.001 |
| Prior Bypass | |||||
| Amputation or death | 74.2 | 62.9 | <0.001 | 0.8 (0.78-0.9) | <0.001 |
| Mortality | 65.9 | 51.2 | <0.001 | 0.79 (0.7-0.9) | <0.001 |
| Major amputation | 25.2 | 23.4 | 0.001 | 0.87 (0.78-0.97) | 0.013 |
| Revascularization | 63.2 | 50.5 | <0.001 | 0.7 (0.7-0.8) | <0.001 |
Back to 2023 Posters


