Clinical Characteristics and Cardiac Physiology of Mechanical Pulmonary Thrombectomy
Samuel D Leonard, Mitchell George, Gregory Estrera, Charles C Miller, III, Stuart D Harlin
McGovern Medical School at UTHealth, Houston, TX
INTRODUCTION: Pulmonary embolism (PE) is the third most common cause of cardiovascular death affecting nearly 100,000 patients annually in the United States. Reported mortality related to acute PE and its sequelae ranges from 10-30 percent. The Inari FlowTriever mechanical thrombectomy system was recently approved for pulmonary mechanical thrombectomy (PMT); however, there is limited data related to perioperative alterations in cardiac physiology in patients undergoing percutaneous thrombectomy. We present the largest single institutional review our clinical and technical experience with PMT among low, intermediate and high-risk pulmonary emboli. METHODS:We performed a multicenter retrospective analysis of patients with acute and chronic pulmonary embolism treated with PMT using the Inari FlowTriever across eleven hospitals with significant patient demographic heterogeneity within the Memorial Hermann Health System from December 2019 through August 2021. Relevant demographics, medical conditions, anatomical characteristics, intra- and postoperative courses, and adverse events were captured for Wilcoxon, paired t test and ANOVA statistical analysis. Biomarkers were log transformed for parametric analysis. RESULTS:We identified 77 patients (age 61±16 yr, 54% female), within the analyzed time period who underwent PMT with 100% technical success rate and complete data were available for 73. There was one post procedure death related to COVID-19 sequalae, and one postoperative myocardial infarction. As suspected, increased incidence of pre-operative right heart strain (RHS) was detected with transthoracic echocardiogram or computed tomography angiograph in patients with higher clot burden (unilateral 7/11 (64%), bilateral 34/36 (94%), saddle 25/26 (96%), P<.01). B-type natriuretic peptide (BNP) was not statistically associated with presence of RHS, though troponin was higher in RHS 0.145, (IQR 0.02 - .62) vs 0.02 (IQR 0.02-0.02), p<0.026). Log troponin increased with higher clot burden (ANOVA p<0.027). No significant difference in preoperative mean PAP, or change in PAP post-procedure, was identified as a function of clot burden; however, mean PAP improved significantly across all those treated (-8mmHg±8.57 overall, p<0.0001) . The greatest mean PAP improvements were seen in those with pre-operative RHS (-11.8±8.6 vs -3.0±2.6, p<0.026). CONCLUSIONS:PMT appears an effective treatment methodology for PE as evidence by immediate hemodynamic improvement, low associated mortality, and minimal perioperative complication rate. Potential advantages include avoiding thrombolytics or post procedure ICU required bedding and improvement in cardiac physiology across multiple levels of PE severity, especially in the setting of RV strain; however long-term follow-up needed to further examine associated benefits. 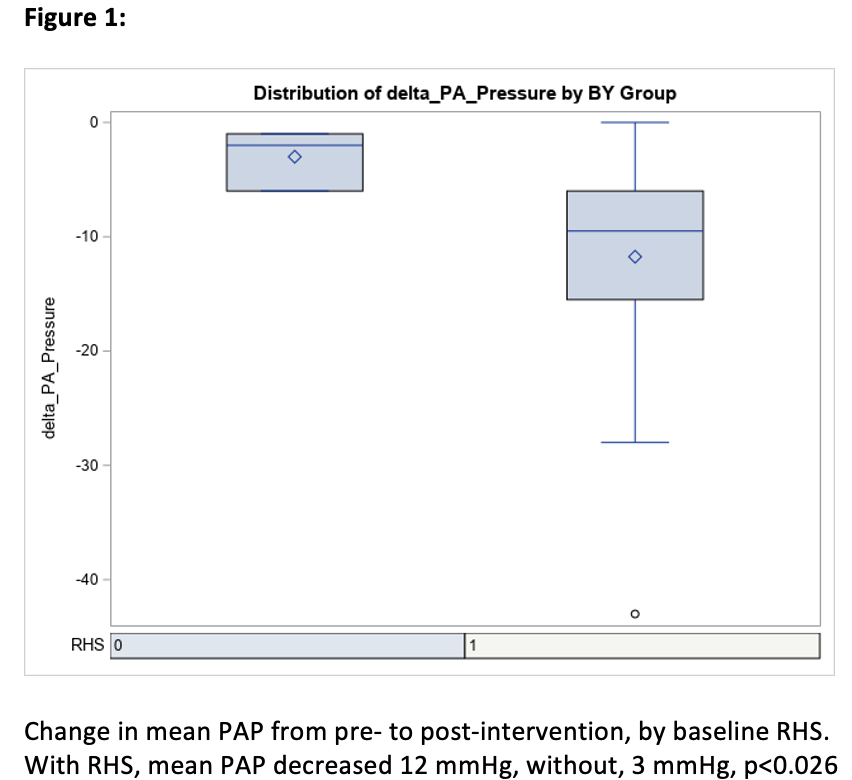
Back to 2023 Display Posters


