Complementary Role of Magnetic Resonance Imaging and Computed Tomography Angiography in Evaluating Acute Type B Aortic Dissection
Maria Katsarou, Ponraj Chinnadurai, Alan B Lumsden
Houston Methodist Hospital, Houston, TX
INTRODUCTION: Treatment of acute type B aortic dissection (aTBAD) largely depends on the presence of clinical symptoms, malperfusion, or rupture. Although in most cases there is a clear indication for treatment, sometimes patients fall into a “grey zone” when the dangers of treatment in the acute phase need to be balanced against potential end-organ damage or future complications. In those cases, accurate diagnosis is paramount for patient risk stratification and directing optimal therapies. Computed tomography angiography (CTA) is the primary imaging modality for the diagnosis and treatment planning for aTBAD. Although magnetic resonance imaging (MRI) has been shown to provide patient-specific aortic hemodynamic information, it is not yet adopted in clinical routine, and is performed in select aortic centers.
The objective of this study was to compare MRI and CTA findings in the setting of aTBAD and report the yield in terms of aortic morphology and hemodynamics.
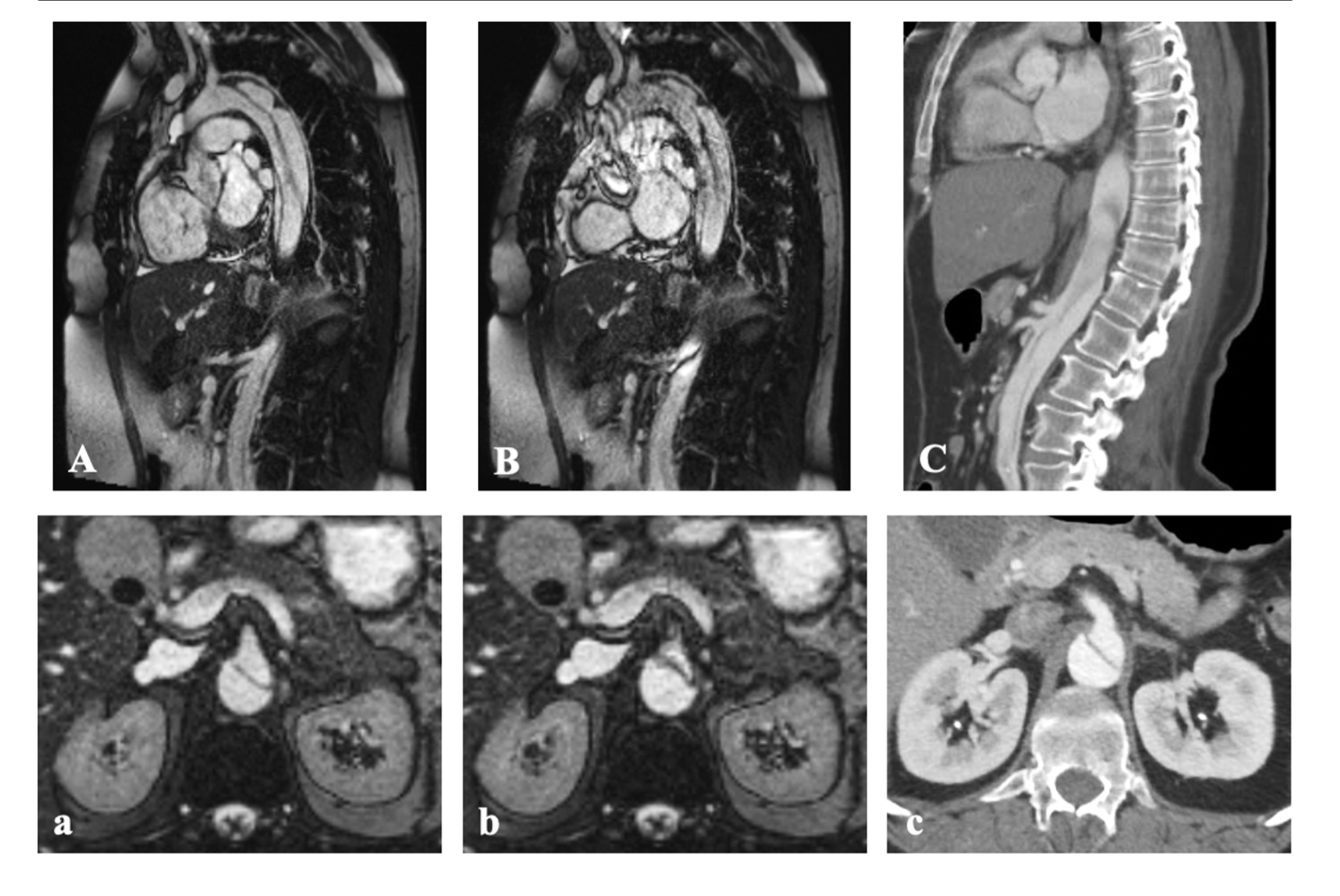
METHODS: A retrospective chart review of all patients diagnosed with aTBAD and who underwent both CTA and MRI studies in the hyperacute and acute phases was performed. Patient demographics and clinical presentation was documented. Image analysis was performed after CTA (non-gated) and MR (cine, TWIST, T1-VIBE sequences) were co-registered using a commercially available software (MM-Oncology workflow, syngo.via®, Siemens Healthineers). Aortic diameters were measured using multi-planar reconstructions. Entry tear location, septal fenestrations, true/false lumen morphology, and visceral vessel patency were assessed during comparative image analysis.
RESULTS: Between January 2016 and March 2022, out of 91 patients with aTBAD, 18 underwent both MRI and CTA imaging, within a median of 1 day (IQR:0.75-2) between two modalities. Mean (±SD) age was 53.3±15.2 years, 9 (50%) were males. Median creatinine (mg/dL) was 1.1 (IQR: 0.90-1.53) and lactate (mmol/L) was 1.3 (IQR: 1.05-1.75). Six/18 (33.3%) had obvious signs of end-organ malperfusion, while the remaining had clinical symptoms that prompted indication for MRI.
Mean proximal, distal, and maximum aortic diameters were 28.2±4.9 vs 27.6±4.9 (p=0.12), 21.0±4.6 vs 20.5±4.2 (p=0.31), and 36.0±7.1 vs 35.3±7.2 (p=0.003) mm for CT and MR accordingly (Figure 1). Mean difference in aortic diameters was 0.6±0.9 mm (p<0.001) . Mean number of fenestrations was 1.9±0.8 vs 1.9±1.1 (p=0.86), whereas false lumen thrombus, morphology and extent of dissection were equivalent between two modalities in the acute setting. In 7/18(38.9%) patients, findings regarding origin of visceral vessel from true/false lumen (n=6) and patency (n=2) were discordant between two modalities (Figure 2).
CONCLUSIONS: Comparative analyses of MRI and CTA datasets in the setting of aTBAD, showed equivalent aortic morphometric findings with <1 mm mean difference between the two modalities. Dynamic and time-resolved MRI provided additional data concerning dynamic obstruction of visceral vessels and false lumen flow dynamics that might be relevant for selecting patients for optimal treatment. 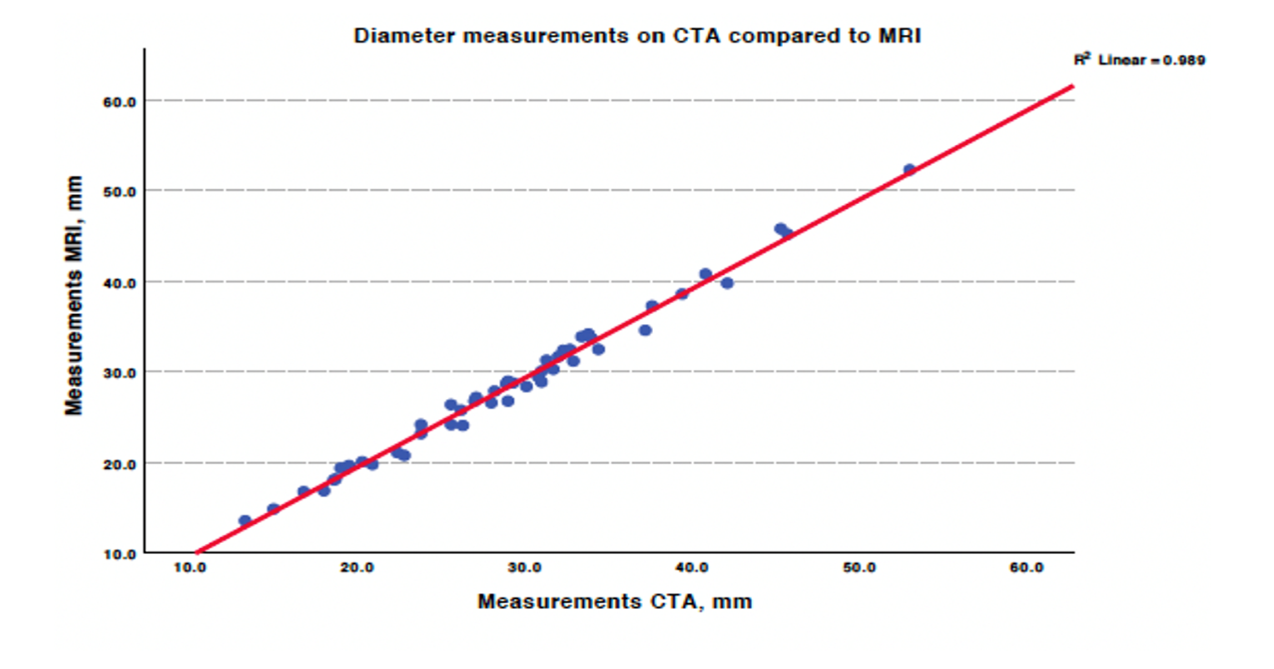
Back to 2023 Display Posters


