Safety and efficacy of vertebral artery transposition at the time of thoracic aortic endovascular repair
Kaitlyn Marie Dunphy1, Matthew Cabrera1, Javairiah Fatima1, Misaki M Kiguchi1, Steven D Abramowitz1, Raghuveer Vallabhaneni2
1MedStar Health, Washington, DC;2MedStar Health, Baltimore, MD
Background: Vertebral artery transposition (VAT) is an infrequently performed procedure for vertebrobasilar insufficiency due to limited data endorsing its use. However, in the setting of aberrant aortic anatomy, vertebral artery transposition is used to preserve dominant vertebral flow in patients who require coverage of the ostium with stent graft repair. There is sparse data discussing the safety and effectiveness of vertebral artery transposition to preserve posterior circulation in this setting.
Methods:All patients who underwent thoracic aortic endovascular aneurysm repair (TEVAR) from 2014-2020 were queried in our hospital system. Those who underwent VAT within thirty (30) days either before or after TEVAR were included in the study. Nine (9) patients met the above criteria and were retrospectively reviewed for safety and efficacy.
Results:All 9 patients (100%) who underwent VAT achieved immediate technical success. The indication for vertebral artery transposition in all patients was aberrant vertebral anatomy with plans for stent graft coverage of its native origin. All patients had a concomitant subclavian artery revascularization either with carotid subclavian bypass or with carotid subclavian transposition. 5 of 9 (55.6%) were also performed with concomitant TEVAR, 4 of 9 (44.4%) were performed as part of a staged aortic repair. 6 of 9 (66.7%) of patients experienced post-operative complications and 2 of these were cervical or cranial nerve injuries. Patients who suffered from cervical or cranial nerve injuries had a statistically significantly higher body mass index (BMI) compared to those who did not suffer nerve injury. 7 of 9 patients underwent post-operative surveillance imaging with either CT angiography or duplex ultrasound within six (6) months of VAT and all 7 patients were noted to have patent conduit at the time of imaging. 0% of patients experienced clinically evident cerebrovascular accident (CVA) within thirty (30) days.
Conclusion:VAT is a safe and effective procedure in the setting of aberrant anatomy and need for TEVAR. Given its limited indication, this is a difficult procedure to study as few of these are performed annually. While cranial and cervical nerve injury is a concern in vertebral revascularization, this may be associated with patient BMI and should be taken into consideration with surgical planning. 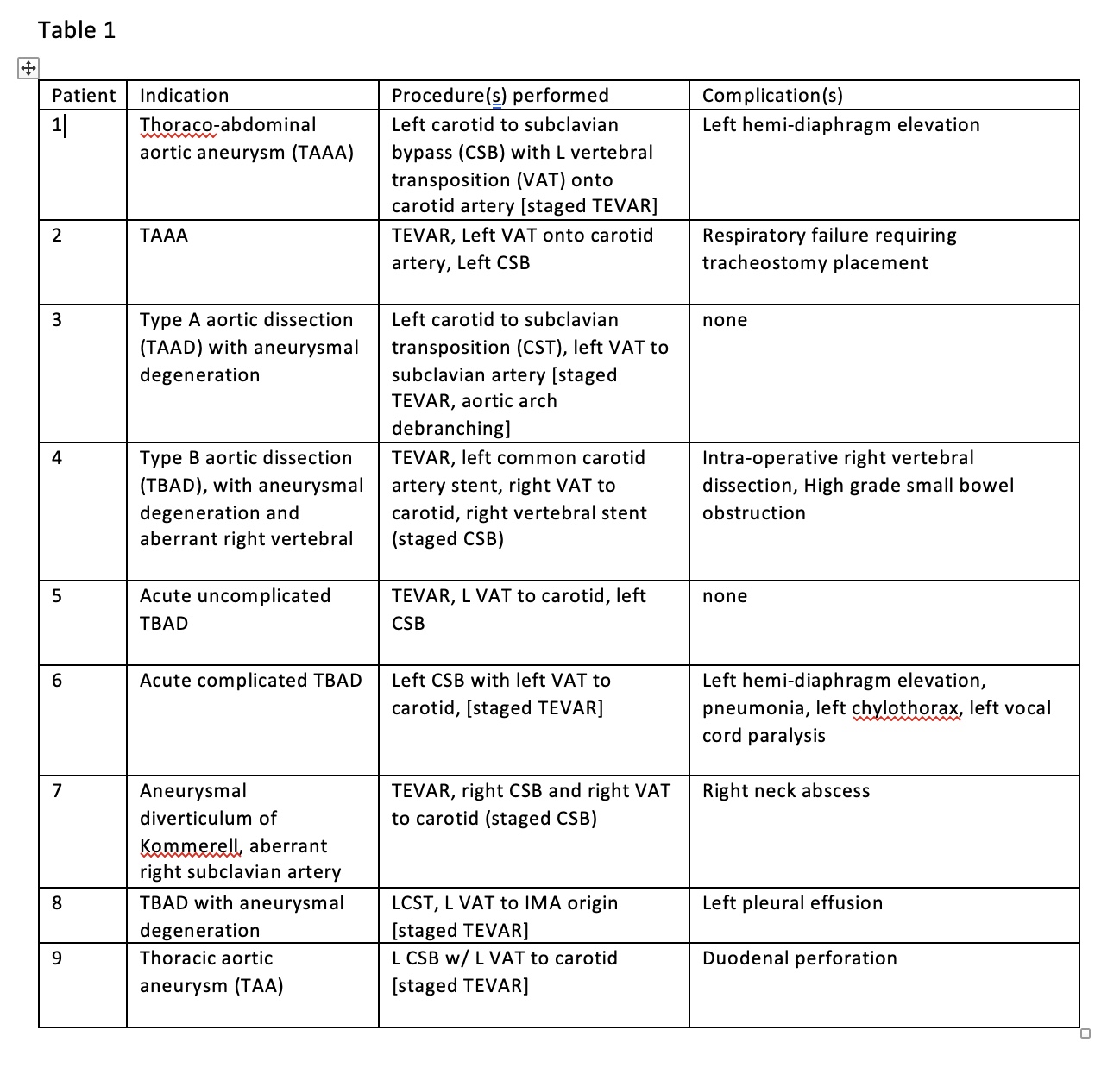
Back to 2023 Display Posters


