Post-Operative Urinary Retention after Endovascular Aortic Aneurysm Repair in a Veteran Population
Sally Boyd, Diana Otoya, Douglas Hogan, Wayne Tse, Kedar Lavingia, Michael F Amendola
VA Medical Center/VCU, Richmond, VA
BACKGROUND:
Post-operative Urinary retention (POUR) is a common multi-factorial post operative complication which has been associated with increase length of stay, risk of urinary tract infection, reduced ambulation and increased need for rehabilitation. Predisposing POUR factors include age, sex, fluid management, type of operation and anesthesia. History of benign prostatic hypertrophy (BPH) and other urological cancers have also been implicated. Previous research has postulated that disruption of pelvic circulation and/or iliac artery manipulation as possible contributors while others argue a more neurogenic component. We set forth to examine POUR in a veteran population undergoing EVAR.
METHODS:
All patients who underwent elective EVAR at a single Veterans Affairs Medical Center from January 2010 to December 2021 were included. Patient characteristics and clinical data such as age, body mass index, comorbidities, smoking status, anesthesia type, operating time, proximal EVAR graft diameter, distal iliac graft diameters, if hypogastric embolization was undertaken, length of stay, post-operative complications, date of death, benign prostatic hypertrophy (BPH) diagnosis, and diagnosis of bladder and/or prostate cancer. Post-operative outcomes for patients who experienced urinary retention (UR) were compared to no urinary retention (non-UR) utilizing student t test*, Fishers exact**, and multivariate analysis.
RESULTS:
A total of 241 patients under EVARs at our institution. Twenty patients (8.3%) experienced urinary retention in the post-operative period. The percentage of hypogastric embolization (22.6% vs. 20%; p=0.79*) was not significantly different between the UR and non-UR groups respectively. The percentage of bladder/prostate diagnosis (17.2% vs. 30%; p=0.16*) was higher in patients with POUR but not statistically significant. BPH diagnosis (15.8% vs. 25%; p=0.03*), post operative acute kidney injury (3.6% vs. 15%; p=0.02*), length of stay (2.6 vs. 4.5; p=<0.01*) and readmission rate (8.1% vs. 30%; p=<0.01*) were statistically significant between the UR and non-UR groups respectively. Additionally, 100% UR patients underwent general anesthesia compared to 93.2% non-UR (p=0.48*). There was no significant difference in the patient comorbidities except lower rate of hypertension in the UR compared to the non-UR group (65% vs 82.8%; p=0.05*). Using Department of Veterans Affairs Managerial Cost Accounting Office (MCA) Cost per Treating Specialty 2019 Report, average cost of inpatient vascular department bed was estimated to be $5,727.42 ± 215.83 per day. An additional 2 days of inpatient stay would result in an increased $11,454.84 for urinary retention.
CONCLUSIONS:
In our analysis, we found approximately 8.3% incidence of post-operative urinary retention with a statisticallysignificant increase in length of stay, readmission rates and post operative acute kidney injury. These data emphasize the importance of post operative surveillance in patients with history of BPH who are at risk for POUR and should encourage increased vigilance for foley management to prevent possible prolonged more insight on timing of foley removal to prevent longer length of stay and readmission in EVAR patients. 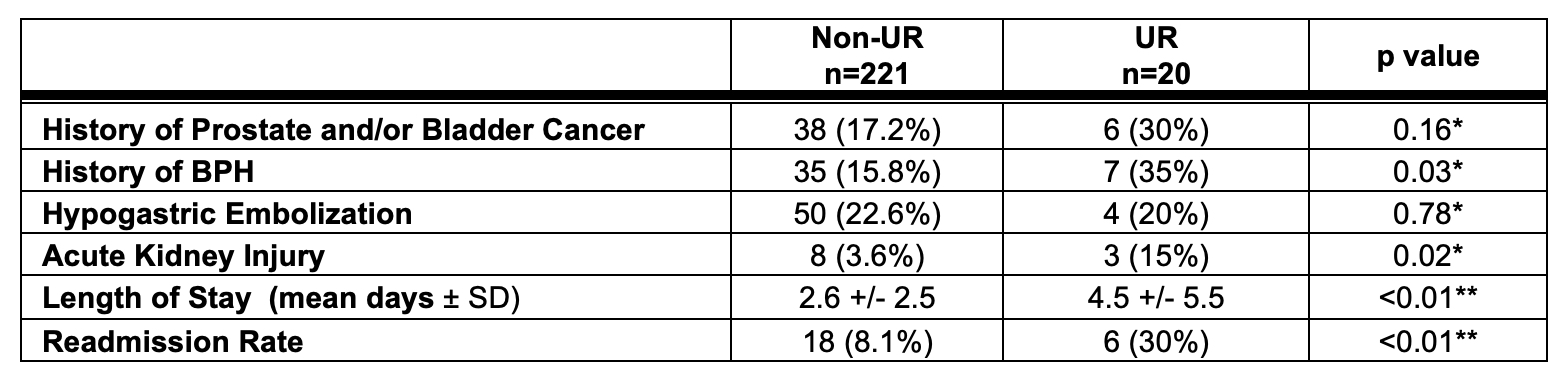
Back to 2023 Display Posters


