Back to 2024 Posters
No Sex Disparities after Abdominal Aortic Aneurysm (AAA) Repair: A Propensity Score Analysis of a Retrospective Single Center Cohort
Yetzali Claudio-Medina, Houssam Farres, Hennessy Morales Arroyo, Christopher Jacobs, Camilo Polania Sandoval, Young Erben
Mayo Clinic, Jacksonville, FL
BACKGROUND: Abdominal aortic aneurysms (AAA) can present with abdominal or lumbar pain or as an incidental finding as they can be asymptomatic, being more common in male compared to female patients. The wide implementation of endovascular aneurysm repair (EVAR) over open aortic repair (OPEN) for both non-ruptured and ruptured AAA have allowed for lower mortality rates and length of hospital stay for patients. However, an equal distribution of outcome improvements has not been observed between sexes.Female patients have been found to have higher peri- and post-operative risks and complications throughout AAA repair. Overall, female patients are more likely to have higher complication and mortality risk than their male counterparts after undergoing both OPEN and EVAR; but are especially higher following EVAR. Furthermore, due to a lower proportion of female patients presenting and being diagnosed with AAA and the differing qualifying criteria for AAA repair, female patients may be often excluded from studies that could have aided in the development of a better standard of care for them. Thus, further understanding of the comorbidities and risk factors in female patients associated with unequal outcomes compared to male patients following both OPEN and EVAR are needed. This study aims to identify factors that may contribute to greater risk and complication rates in female patients as well as how the short- and long-term outcomes compare between sexes following both OPEN and EVAR.
METHODS: Study design: A single-center retrospective cohort study was conducted between 2002 and 2024. We included adult patients who underwent open (OPEN) or endovascular (EVAR or fenestrated-EVAR) AAA repair at our institution. Our Institutional Review Board (IRB) approved this project (IRB# 24-004735). Patient consent was waived due to the study's retrospective nature and the subjects' lower-than-minimal risk.Patients who underwent AAA repairs were identified from the electronic medical records. Those who had thoracoabdominal or iliac aneurysms and those whose primary AAA repair procedure was outside of our institution were excluded from the study. Patient demographic information, comorbidities, aneurysm details, surgical variables, short- and long-term untoward events were collected. Comorbidities included for analysis are as listed in the Society for Vascular Surgery practice guidelines and include hypertension, diabetes mellitus, hyperlipidemia, smoking history, chronic kidney disease, chronic obstructive pulmonary disease, coronary artery disease, atrial fibrillation, and stroke. A distinction was made between EVAR and FEVAR because of the increased complications associated with the use of fenestrated grafts.
Measures: The primary outcome was all-cause mortality. Secondary outcomes were 30-day, and long-term complications. 30-day complications included any event outside of the normal postoperative course (e.g., bleeding, wound complication, postoperative atrial fibrillation, acute kidney injury, ileus, pneumonia, pseudoaneurysm, and mortality) and any other complication from discharge to 30 days after the procedure (i.e., wound complication, graft/limb thrombosis, deep venous thrombosis (DVT), endoleak other than type II, and bowel obstruction). Long-term complications included any complication related to the index procedure such as: wound complications occurring after 30-days, graft thrombosis/infection, endoleak other than type II, pulmonary embolism, and aneurysmal sac growth. Type II endoleak was not considered a complication due to its relative benign nature if combined without aneurysm sac growth. Re-intervention was defined as any additional procedure to treat infection, thrombosis, endoleaks, and further aneurysmal degeneration proximally or distally. Potential confounders for the analysis included age and type of procedure. Other confounders were not addressed as they were not observed to be significantly different among male and female patients.
Analysis: Statistical analysis was performed using R® v.4.4.1. Normal distribution was ascertained by the Shapiro-Wilk test. The categorical variables were analyzed using Pearson’s Chi-squared test, and continuous variables with non-parametric distribution were analyzed using the Mann-U-Whitney test. A p-value of <0.05 was considered statistically significant. A 4:1 propensity score matched cohort was obtained using age and type of procedure. Survival analysis was conducted between both sexes in terms of the primary and secondary outcomes. Log-rank test was used to ascertain differences in the survival analysis. Data was obtained and audited before analysis to reduce information bias. All information was collected sequentially in an encrypted database to ensure patient confidentiality of personal information, reducing the risk of information and selection bias by retrieving the information as needed. This work follows the STROBE criteria.
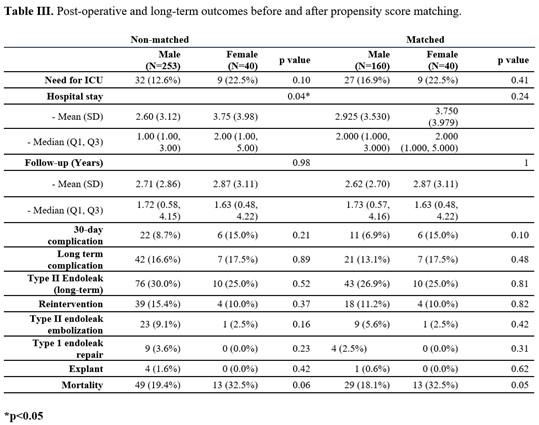
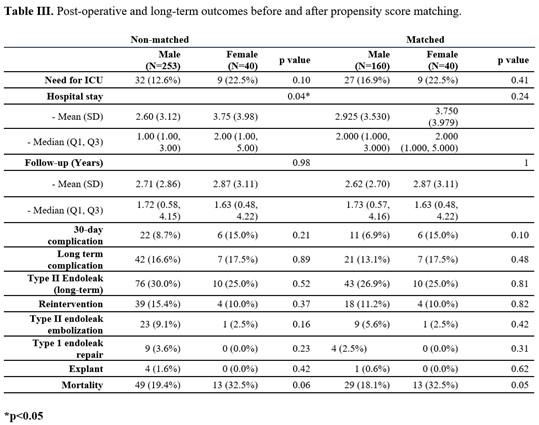
RESULTS: A total of 293 patients who underwent EVAR (n=232), FEVAR (n=33), or OPEN (n=28) AAA repair were included. There were 40 (13.7%) female and 253 (86.3%) male patients with a mean age of 74.1 ± 10.4 and 74.4 ± 8.3 years, respectively. There were no differences in the proportions of patients with hypertension, diabetes, hyperlipidemia, smoking history, chronic kidney disease, chronic obstructive pulmonary disease, coronary artery disease, atrial fibrillation, or prior stroke. After 4:1 propensity score matching was completed, there were 40 (20%) female and 160 (80%) male patients. After matching, hypertension was more prevalent in female than male patients (92.5% vs 77.5%;
P= 0.03)
(Table I). For the matched cohort, the proportion of patients with infrarenal aneurysms was 81.9% for male and 82.5% for female patients (
P= 0.92). The remaining ones had juxta- or pararenal AAA. Saccular aneurysms were present in 16.9% of male and 25% of female patients, whereas fusiform aneurysms in 83.1% and 75%, respectively (
P= 0.19). Ruptured AAA was present in 1.9% of male, and none in our female cohort (
P= 0.38). The mean size of the AAA at the time of intervention was found to be smaller in our female cohort before (51.3 ± 7.0mm vs 53.9 ± 9.0mm;
P= 0.02) and after matching (51.3 ± 7.0mm vs 54.2 ± 9.1mm. P=0.02). Before matching, female patients were found to be more likely to present with symptoms (25.0% vs 12.3%;
P= 0.03) but this difference was not significant after matching (25.0% vs 13.8%;
P= 0.08),
Table II. Before matching, female patients had significantly longer hospital stays (3.8 ± 4.0 days vs 2.6 ± 3.1;
P= 0.04), and after matching, this difference was similar between sexes (3.8 ± 4.0 vs 2.9 ± 3.5;
P= 0.27). The need for intensive care unit (ICU) care was not statistically significant before (22.5% vs 12.6%;
P= 0.10) or after matching (22.5% vs 16.9%;
P= 0.41). Mean follow-up duration was 2.7 ± 2.9 years for the entire cohort. 30-day (6.9% vs 15.0%. p=0.10) and long-term complications (13.1% vs. 17.5%. p=0.48) although were more prevalent in our female cohort, this was not statistically significant. Type II endoleak rates were 26.9% for males and 25.0% for females (p=0.81). Re-intervention rates were 11.2% for male and 10.0% for female patients (p=0.82). All-cause mortality was no different among sexes (32.5% vs. 18.1%, p=0.05),
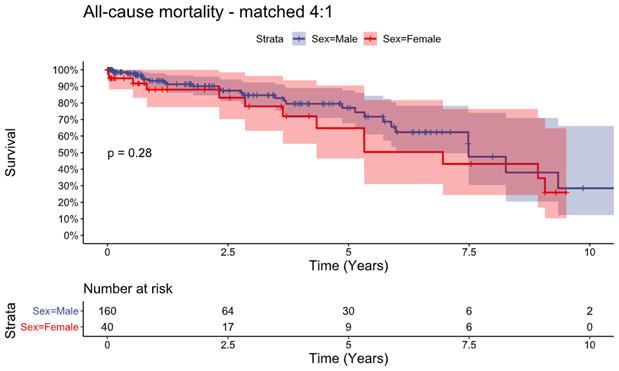
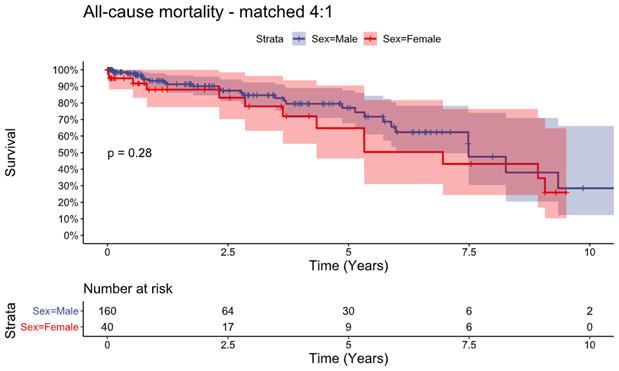
(Table III). Survival analysis of all-cause mortality is shown in
Figure 1 and there was no difference.
CONCLUSIONS: Despite a smaller aortic size, female patients present more frequently with symptoms related to AAA. After propensity score matching, their outcomes however are comparable to that of their male counterparts.
Back to 2024 Posters