Back to 2024 Posters
Carotid Artery Intervention May Still Be Justified In Asymptomatic End-Stage Renal Disease Patients
Junji Tsukagoshi, Neha Sunkara, Mitchell W Cox
University of Texas Medical Branch at Galveston, Galveston, TX
Intro & Background:While carotid endarterectomy (CEA) and stenting have both proven to be beneficial in multiple trials, patients with a short life expectancy or multiple medical comorbidities may not derive much benefit from these interventions. Patients with end-stage renal disease (ESRD) represent such a group. The benefits are especially questionable for asymptomatic carotid artery disease and these patients may not be ideal candidates for intervention. We have utilized large administrative data to assess real-world outcomes of carotid intervention in the ESRD population.
Methods: Using TriNetX Data Network, a global federated database of over 250 million patients, a retrospective cohort study of patients up to July 2024 with and without ESRD who underwent CEA or stenting for asymptomatic carotid artery disease was conducted. Eligible patients were 1:1 propensity score-matched for preoperative co-variates including demographics, comorbidities, and medications. We calculated and compared the 30-day, one-year, and five-year outcomes of stroke/transient ischemic attack (TIA) and mortality amongst the two cohorts using odds ratio (OR) or hazard ratio (HR) with a 95% confidence interval (CI).
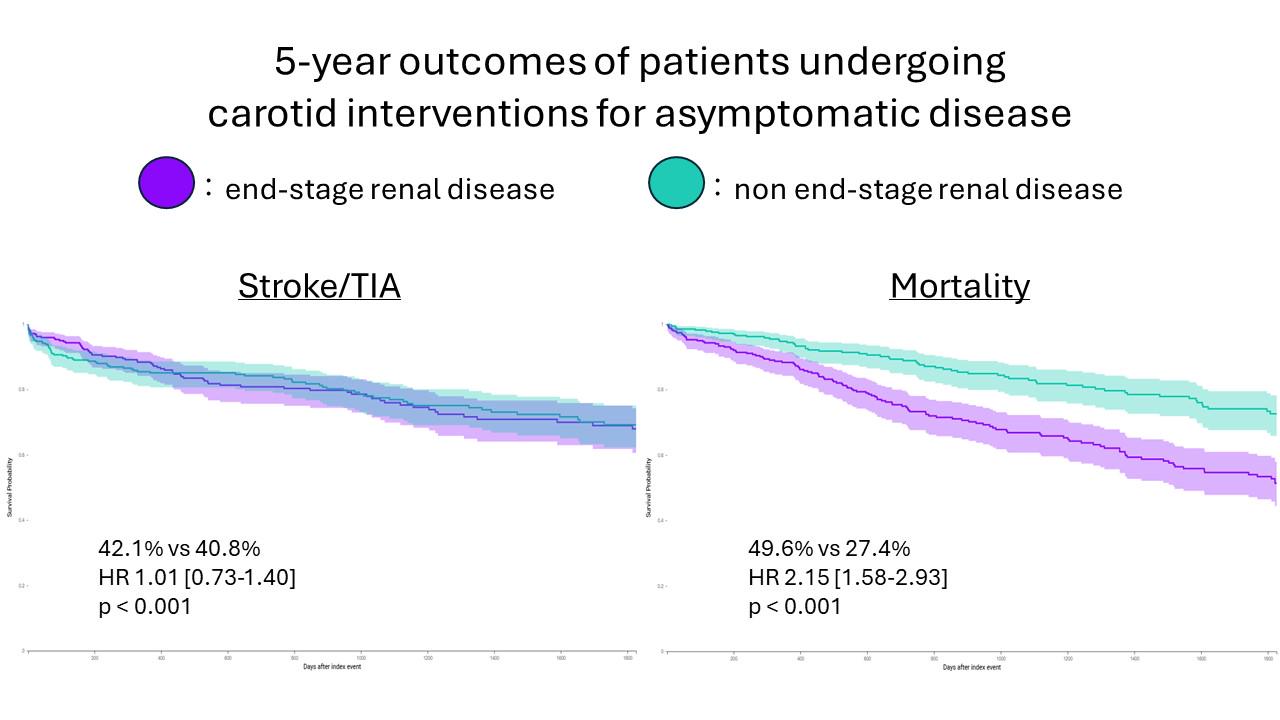
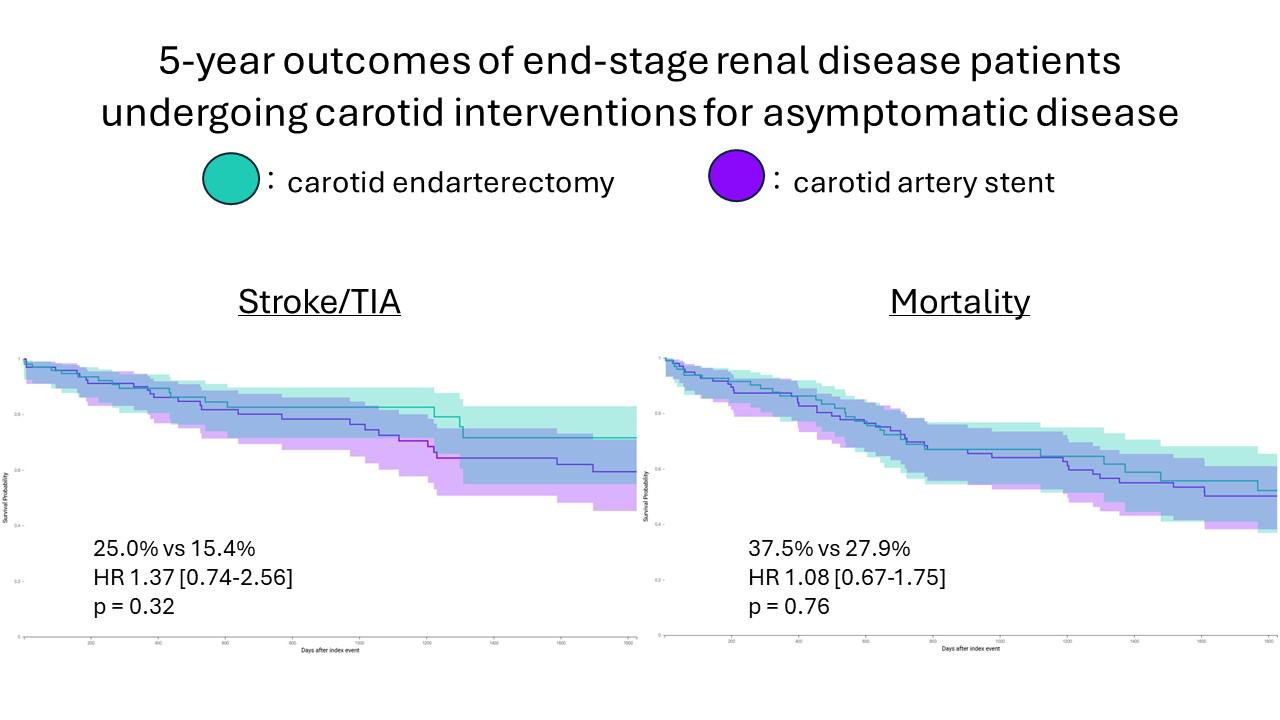
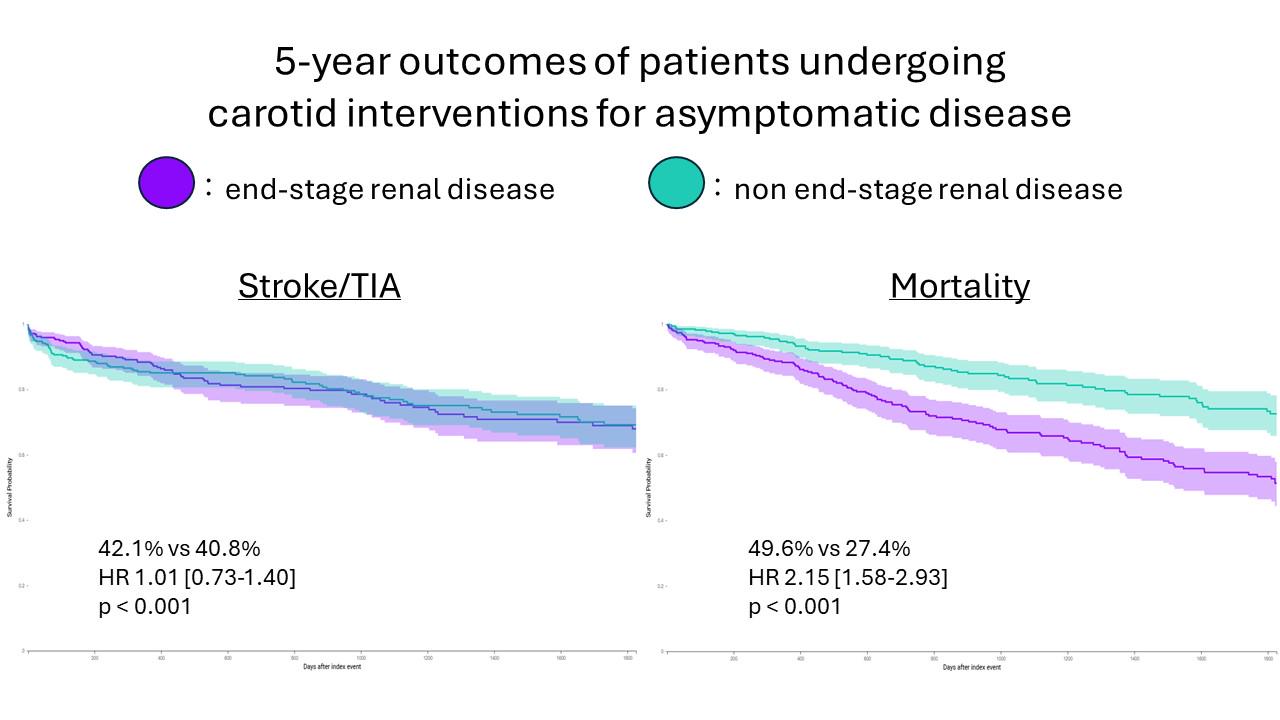
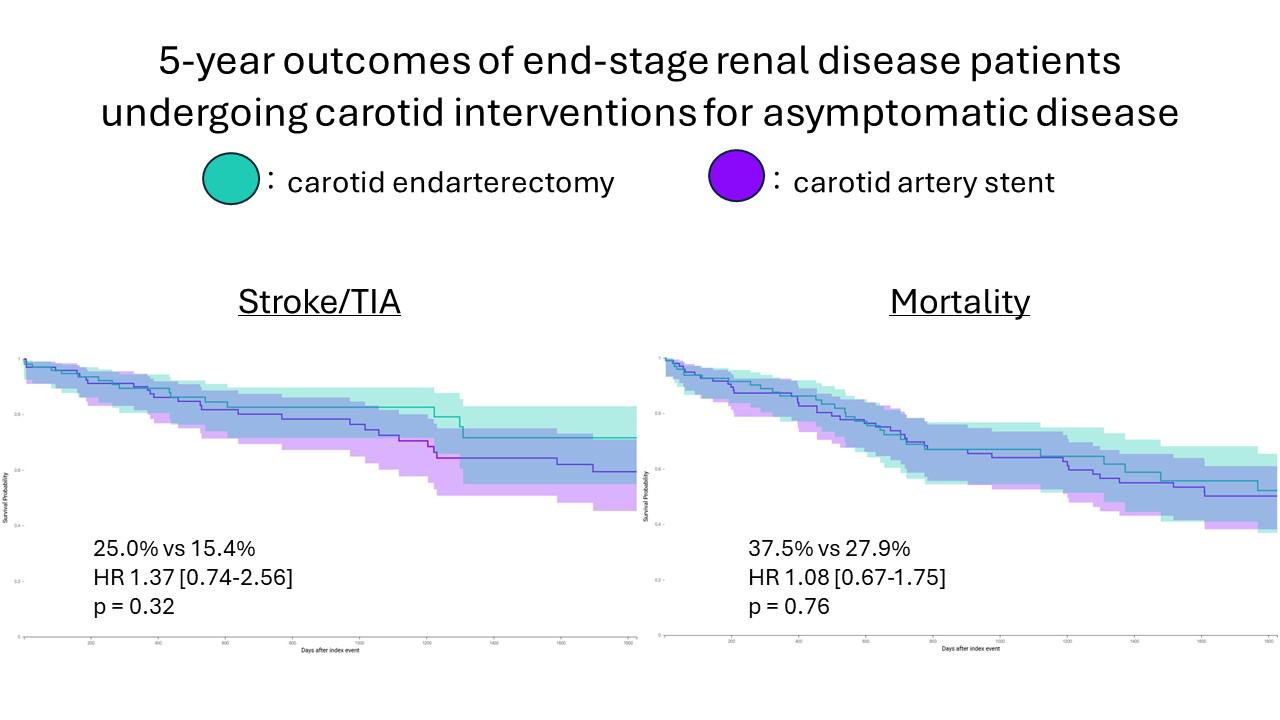
Results:This study identified 351 ESRD patients and 30,730 non-ESRD patients who underwent carotid intervention for asymptomatic carotid artery disease. 348 patients were matched and outcomes up to five years were compared. 53.6% were male with a mean age of 67.3±8.7. Mean follow-up was 986 days. Outcomes at 30 days resulted in comparable rates for stroke/TIA and mortality. The stroke/TIA rate remained comparable out to five years, but mortality was significantly higher in the ESRD group at both one-year (18.7% vs 4.9%, HR [95% CI] = 2.20 [1.24-3.90]) and five years (33.6% vs. 17.5%, HR [95% CI] = 2.15 [1.58-2.93]). Subgroup analysis comparing CEA vs stenting demonstrated statistically similar stroke/TIA rates at all time points, but the 5-year stroke/TIA rate was 25.0% for CEA vs 15.4% for stenting (p=0.14). Likewise, mortality was comparable at time points, but the 5-year mortality was 37.5% for CEA vs 27.9% for stenting (p=0.14).
Conclusion:ESRD patients exhibited nearly twofold long-term mortality after carotid intervention compared to non-ESRD patients, while neurologic benefits remained comparable. In these patients, long-term neurologic complications and mortality remained statistically similar. Despite limitations inherent to large administrative database research, this study highlights the poor prognosis of ESRD patients undergoing carotid intervention and the importance of careful patient selection to justify clinical decision-making.
Back to 2024 Posters