Back to 2024 Posters
Renal Function Mid-Term Outcomes After Complex Endovascular Aortic Aneurysm Repair
Andres V Figueroa, Mira T Tanenbaum, Jose Eduardo H Costa-Filho, Natalia I Coronel, Marilisa Soto-Gonzalez, Mirza S Baig, Greg Modrall, Melissa L Kirkwood, Carlos H Timaran
University of Texas Southwestern Dallas, Dallas, TX
Background: Complex
endovascular aortic aneurysm repair (EVAR) has emerged as the preferred treatment option for most aortic aneurysms. Perioperative renal dysfunction may be reduced by EVAR in complex repairs. Contrast-induced nephropathy, renal microembolization, and acute tubular necrosis, however, contribute to progressive deterioration in renal function after complex EVAR. This study aims to assess renal mid-term outcomes after complex EVAR.
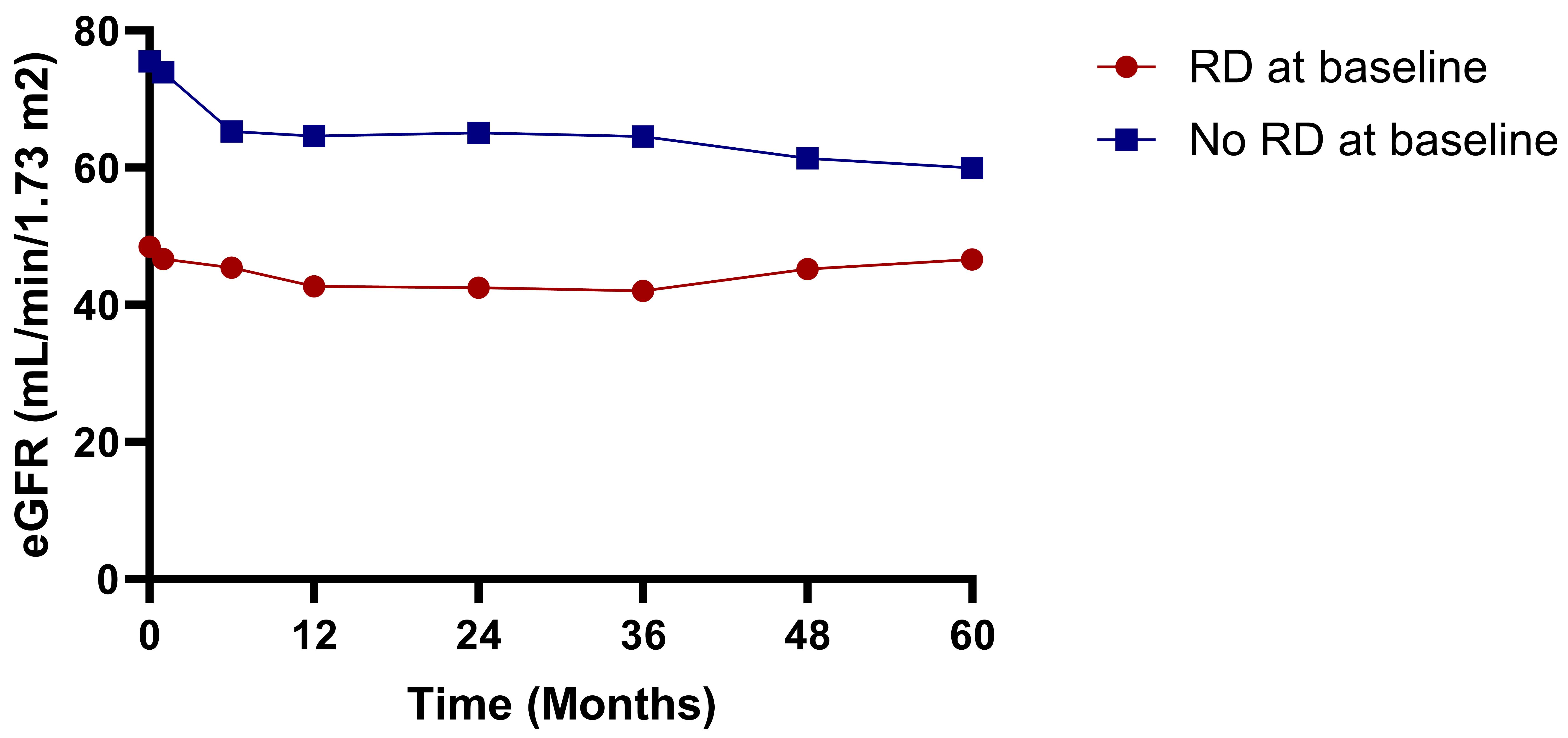
Methods: A retrospective study of consecutive patients undergoing complex EVAR between 2015 and 2023 was performed. Renal function was evaluated using estimated glomerular filtration rate (GFR) at baseline, discharge, 1 month, 6 months, and annually thereafter up to 5 years. Renal dysfunction (RD) at baseline was defined as GFR < 60 ml/min/1.73m
2. The presence of acute kidney injury (AKI), renal artery (RA) thrombosis/stenosis, renal failure requiring dialysis, and progression of chronic kidney disease (CKD) were evaluated. Patients on dialysis at baseline were excluded.
Results: A total of 414 patients underwent complex EVAR (mean age, 73 ± 8 years; 293 male [71%]) with a mean follow-up of 24 ± 21 months. There were 173 patients (42%) with RD at baseline. A total of 824 RAs were stented using 565 fenestrations (68%) and 259 branches (32%). Complex EVAR technical success was 97.3%. Post-operative AKI and dialysis requirements occurred in 55 (13%) and 11 (2.6%) patients, respectively. The mean GFR during follow-up was significantly lower than baseline with a decrease of 18% at 5 years (63 vs. 53 ml/min/1.73m
2;
P =.0022). A significant decrease in GFR was initially observed after 1 year in patients with a history of RD (48.5 vs. 42.69 mL/min/1.73m
2;
P=.0014). In patients without RD, a significant decrease in GFR was initially observed at the 30-day visit (75.5 vs. 73 ml/min/1.73m
2;
P=.003) (Figure). Cumulative CKD stage progression after 1, 3, and 5 years was observed in 110 of 282 patients (39%), 51 of 131 patients (39%), and 24 of 53 patients (45.2%), respectively. AKI was an independent predictor of progression of CKD at 1 year (OR= 14.05, 95% CI [3.11 - 63.40],
P=.001) (Table). Freedom from RA thrombosis/stenosis by Kaplan-Meier estimates was 96%, 93%, and 90% at 1, 3, and 5 years, respectively.
Conclusion: Acute kidney injury was highly associated with CKD progression at one year. Patients with normal preoperative renal function experienced renal impairment more frequently in the early follow-up period, whereas those with preoperative RD were more prone to worsening renal function during mid and long-term follow-up.
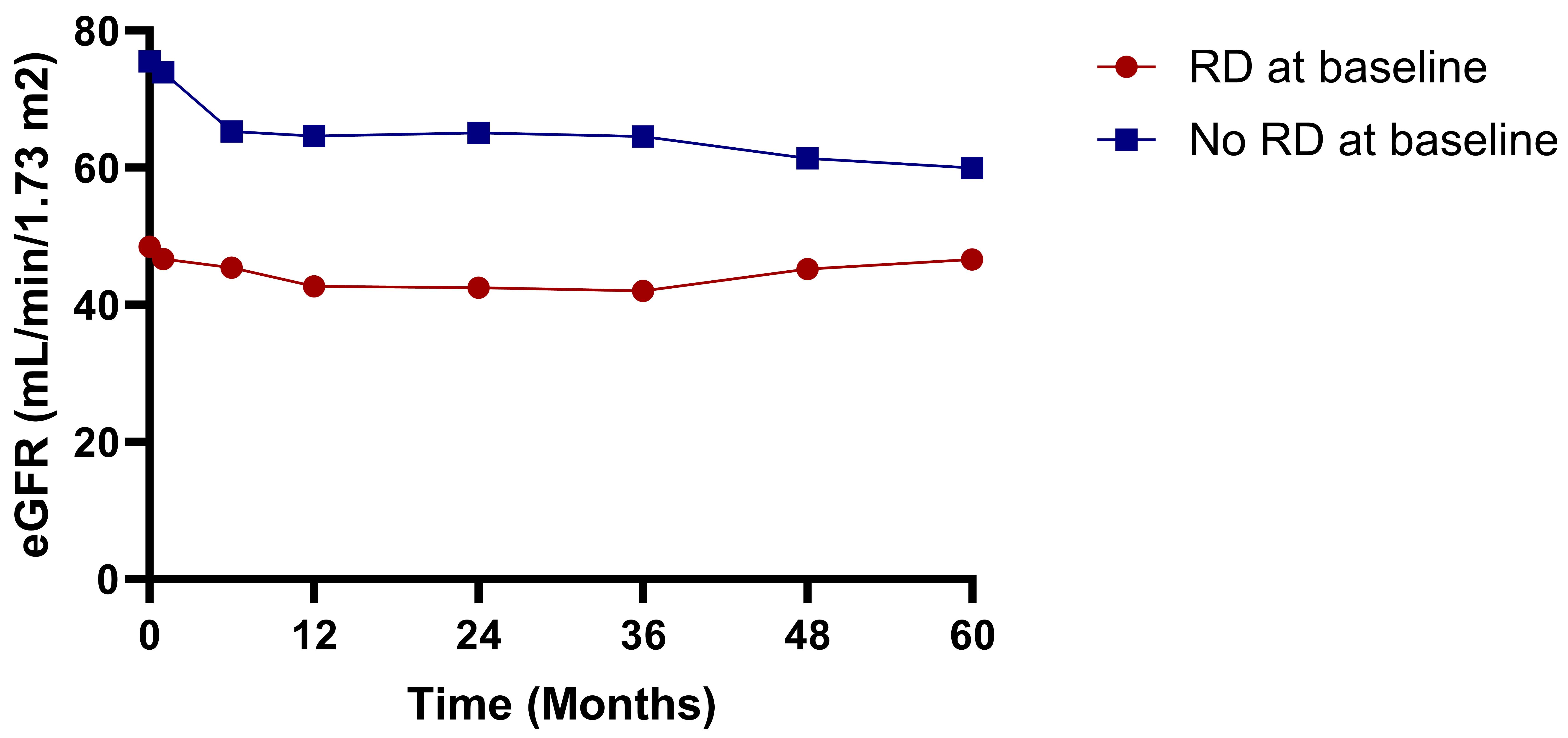
Table I. Logistic regression model for Chronic Kidney Disease progression at 1 year| Variables | Odds ratio | 95% CI | P value |
| Acute kidney injury | 14.05 | 3.1-63.4 | .001 |
| AKI requiring dialysis | .30 | .02-4.72 | .395 |
| RA stenosis/occlusion | 2.14 | .52-8.86 | .291 |
| RA secondary intervention | 1.6 | .32-8.08 | .569 |
| | | |
Back to 2024 Posters