Back to 2024 Posters
Comparative Outcomes of Major Adverse Limb Events in Patients with Peripheral Arterial Disease
Gloria D. Sanin, Elizabeth C. Wood, Ashlee Stutsrim, Timothy K Williams, Kevin Chang, Timothy Craven, Matthew Edwards, Matthew P Goldman
Wake Forest University, Winston Salem, NC
INTRODUCTION: Peripheral arterial disease (PAD) affects up to 20% of individuals over 70. Although PAD is frequently subclinical, its presence is associated with significant morbidity including major adverse limb events (MALE). Despite guideline-directed medical therapy (GDMT) of PAD emphasizing optimal medical therapy (OMT) for PAD, adherence rates to OMT and high-intensity OMT (HIOMT) remain low in many studies. This study aims to evaluate the relationship between OMT, HIOMT, and MALE in the PAD population of a large tertiary medical.
METHODS: We conducted a retrospective analysis of 3471 patients with PAD between 2017 to 2022. OMT was defined as active prescriptions for antiplatelet and statin therapy whereas HIOMT was defined according to the 2016 American Heart Association (AHA) guidelines (antiplatelet and high-intensity statin). Outcomes included the incidence of MALE (defined as above-ankle amputation), all-cause mortality, and need for revascularization. Disease severity (based on WIfi ischemia grades) and other covariates were recorded. Univariable and multivariable proportional hazards regression models were used to evaluate the relationship between predictor variables and outcomes.
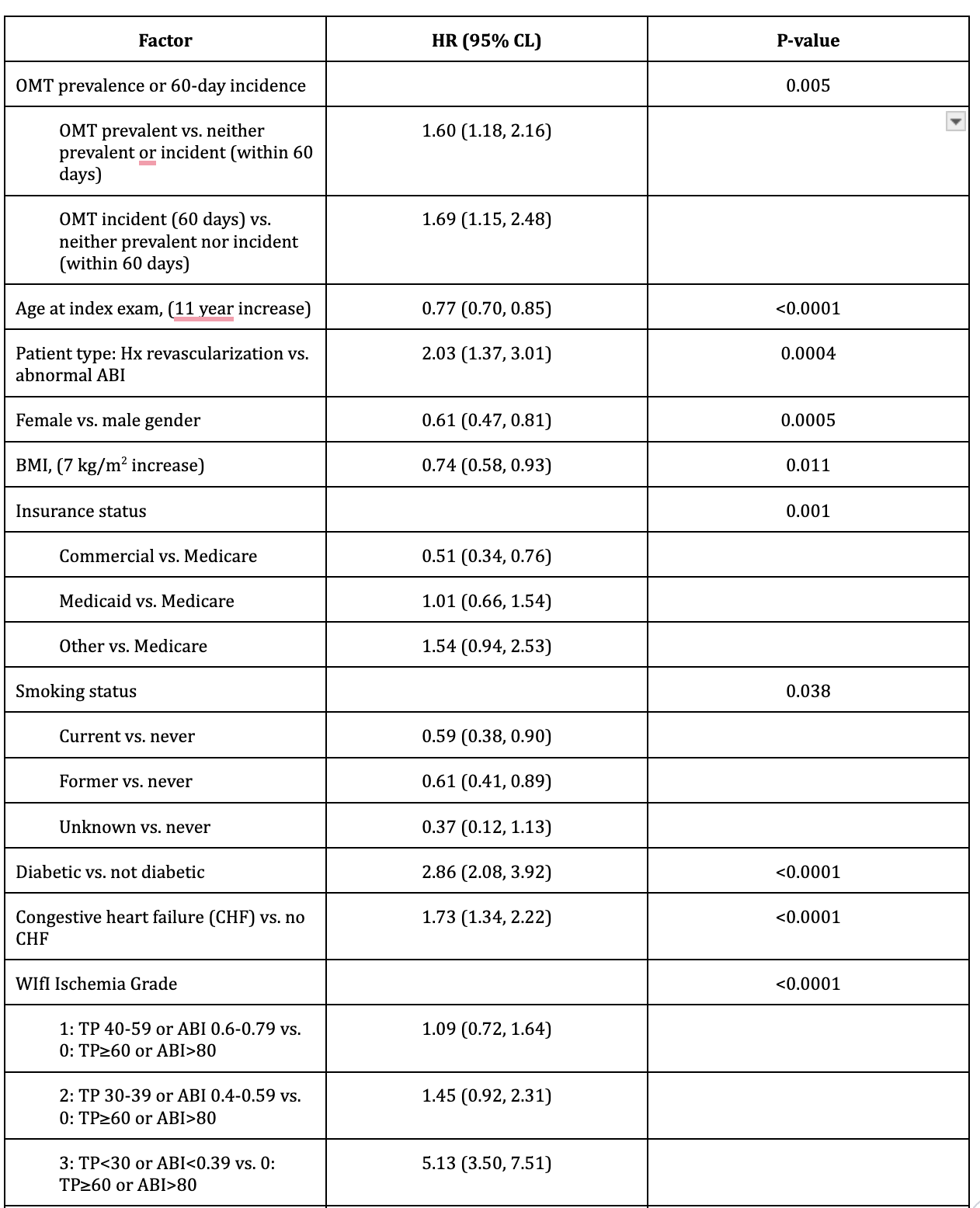
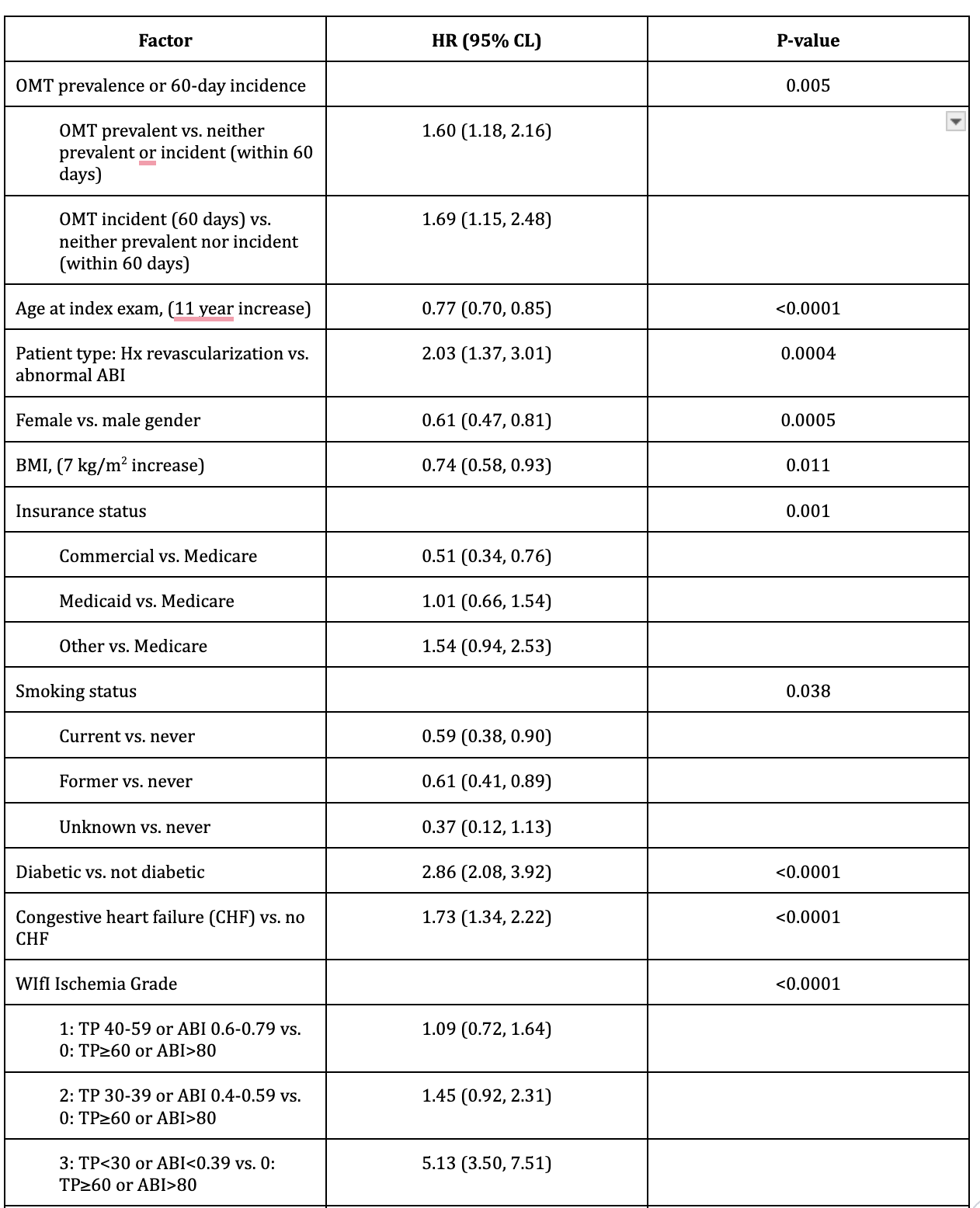
RESULTS: At index vascular study, OMT prevalence was 45.3% and HIOMT 23.6%. The incidence (initiation)/prevalence(continuation) of HIOMT increased to 53.4%, and OMT to 77.1%. MALE occurred in 5.1%. Larger hazard ratios (HR) were observed in patients with prevalent (HR 2.18, 95% CI 1.62- 2.93) and incident OMT within 60 days (HR 2.68, 95% CI 1.85-3.89; p<0.0001) for MALE compared to those without OMT. HIOMT prevalence (HR 1.48, 95% CI 1.13-1.94; p=0.011) was associated with a higher risk of MALE, but not for incident HIOMT with 60 days (HR 1.42, 95% CI 0.92-2.14). Patients with previous revascularization had a higher incidence of MALE compared to those with abnormal ABIs alone (12.5% vs 7%). The WIfi ischemia score showed that patients with more severe ischemia had significantly higher rates of MALE compared to those with less severe ischemia. In multivariable proportional hazards regression, several factors were associated with MALE including WIfI ischemia grade, diabetes, and congestive heart failure (CHF). Table 1.
CONCLUSIONS: Overall, this cohort had low rates of goal-directed-optimal medical therapy in a large, non-random sample of PAD patients. In this sample, goal-directed optimal medical therapy was not associated with decreased adverse limb events over a median follow-up of 3.3 years. As expected, significant associations were found between MALE and traditional risk factors. This highlights the need for earlier recognition of PAD and the institution of GDMT to achieve the previously demonstrated protective benefits of medical therapy.
Table 1. Proportional hazards regression model for major adverse limb events. Results of forward stepwise variable selection procedure (N=3409, 161 events); hazard ratios and 95% confidence limits.
Back to 2024 Posters