Back to 2024 Posters
Feasibility of Building a Markov Model that Represents the Chronic Limb-Threatening Ischemia Patient Journey
Cynthia A Ramazani
1, Adriana Gutierrez
2, Amelia Fogle
1, Yazan Duwayri
1, Manuel Garcia-Toca
1, Nader N Massarweh
3, Katherine McGinigle
4, Emily Spangler
5, Olamide Alabi
1 1Emory University School of Medicine, Atlanta, GA;
2Emory University School of Public Health, Atlanta, GA;
3Atlanta VA Healthcare System, Decatur, GA;
4University of North Carolina School of Medicine, Chapel Hill, NC;
5University of Alabami, Birmingham, AL
BACKGROUND: A new diagnosis of end stage peripheral artery disease, or chronic limb-threatening ischemia (CLTI), is associated with a 25% chance of major amputation in 1 year and 50% chance of death in 5 years, analogous to a cancer diagnosis. Understanding the complex decision-making in CLTI health state transitions can be useful to examine the CLTI journey as it relates to staging and disease progression. We created a CLTI framework to characterize the CLTI journey (Figure 1) and tested its feasibility and ability to fit the CLTI journey of a group of patients with a new diagnosis of CLTI.
METHODS: All patients with an incident CLTI diagnosis undergoing index lower extremity revascularization between June-December 2021 at our institution were reviewed. Patients with major amputations prior to revascularization attempt and those who died between time of CLTI diagnosis (T
d) and index revascularization (T
0) were excluded. Patients were divided into two groups at the time of first follow-up after their first revascularization: those who achieved resolution of their CLTI-defining feature (Group A) and those who did not (Group B). Sociodemographic, preoperative and postoperative antithrombotic medications, revascularization type (open surgical, endovascular, hybrid), Wound, Ischemia, Foot Infection (WIfI) stage, and follow-up data were compared between groups. Event rates for major amputation (M), reintervention (R), and death (D) were estimated. A probabilistic Markov model was constructed to model CLTI-health state transitions and events with a cycle length of three months. Patients were followed for up to 2 years. A
0 was defined as the goal health state (remission) while A
1 was defined as a CLTI disease recurrence after remission achieved. Those with residual CLTI-defining feature after revascularization (Group B) were categorized as stable (B
0), improving (B
1), and worsening (B
2).
RESULTS: Among 228 patients with CLTI newly diagnosed within the study period, 102 limbs (95 patients) remained after the aforementioned exclusions. Mean age was 71.0(10.3) years, 59.8% (n=61) were male, and baseline presentation of CLTI-defining features were as follows: 29.4% ischemic rest pain, 43.1% nonhealing wound, and 27.5% gangrene. Patients underwent open surgical (30.4%, n=31), endovascular (62.7%, n=64), and hybrid (6.9%, n=7) revascularizations during T
0. Major amputation occurred in 17.6% (n=18) of all included limbs.There were no significant differences in age, sex, race, or ethnicity between Groups A and B. WIfI staging was unavailable in 31.4% of limbs secondary to lack of ankle brachial index studies in these patients. Group B had a higher (worse) median [IQR] WIfI stage compared to Group A (3 [2,4] vs 2 [2,2], p=.0013). Major amputation was more common within Group B (22.7% vs. 3.7%, p=.037). Reintervention occurred in 38.2% of limbs and included 46.4% open surgical (n=26), 51.8% endovascular (n=29), and 1.8% hybrid (n=1) procedures. Reintervention was higher in Group B compared to Group A (45.3% vs 18.5%, p=0.026) and time to first reintervention in days was shorter (56 [19,141] vs 222 [168,486], p=.025). Mortality occurred in 18.9% (n=18) of the entire cohort, however, there were no deaths noted during follow up among patients who initially entered Group A after index revascularization. The median time to mortality in days in Group B was 180 [70,406.5]. While there were no differences noted in follow up between Groups A and B, 37.8% of all patients were lost to follow-up during the study periodAll CLTI patient journeys were translated into probabilities of CLTI-health state transitions in our framework (
Table 1). At first follow-up after T
0, there was a 30.8% probability of entering Group A and a 69.2% probability of entering Group B. Only 26.5% of all included limbs entered remission (A
0) initially after index revascularization, with 43.1% (n=44) eventually reaching remission by the end of follow-up.
CONCLUSIONS:The proposed framework characterizes the CLTI journey after revascularization well and can be used to design a Markov model that may aid in complex decision making and test the efficacy of future CLTI interventions. With inclusion of a larger cohort of patients, this model can also be used in conjunction with longitudinal WIfI staging towards the development of a comprehensive staging system for CLTI, similar to that used for malignancy.
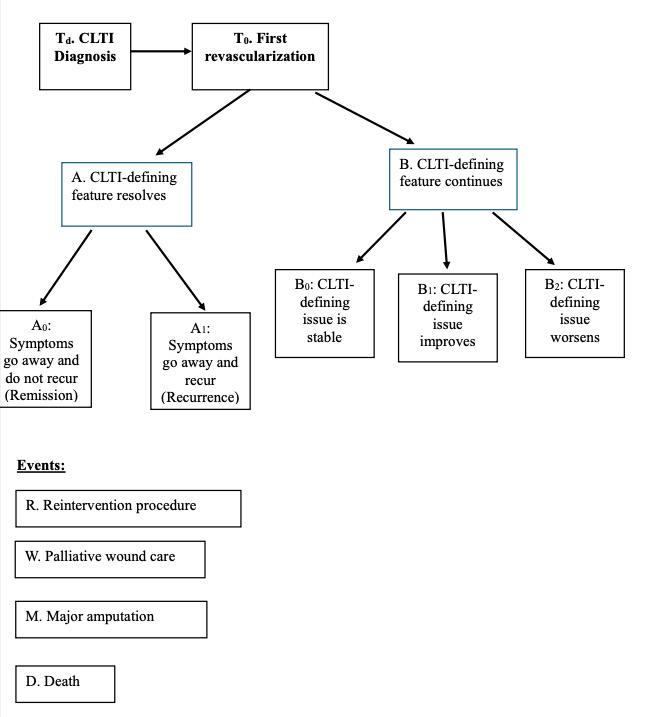
Figure 1: Proposed Chronic Limb-Threatening Ischemia Journey Conceptual Framework for patients undergoing index revascularization.
Back to 2024 Posters
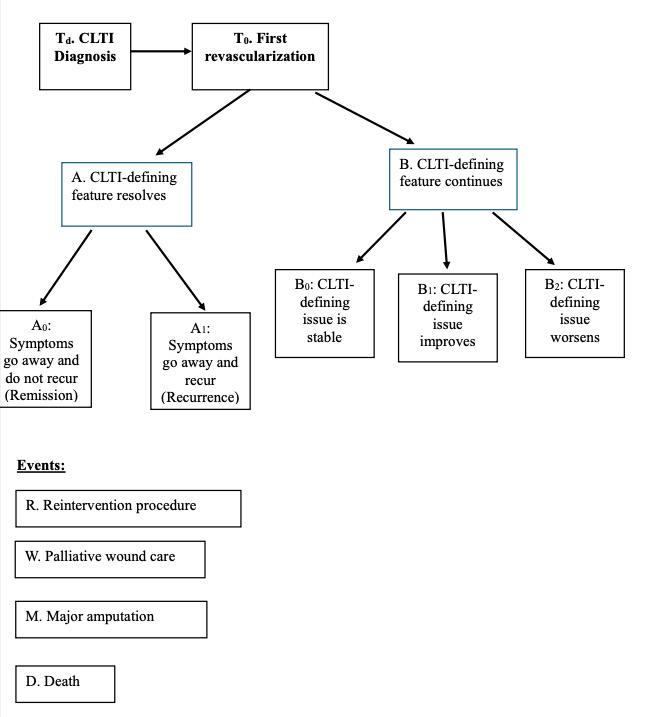 Figure 1: Proposed Chronic Limb-Threatening Ischemia Journey Conceptual Framework for patients undergoing index revascularization.
Figure 1: Proposed Chronic Limb-Threatening Ischemia Journey Conceptual Framework for patients undergoing index revascularization.