Back to 2024 Posters
Glomerular Filtration Rate (GFR) and not sex Highest Predictor of Mortality after Abdominal Aortic Aneurysm Repair: A Cohort Study
Hennessy Morales-Arroyo
Mayo Clinic, Jacksonville, FL
Introduction: Patients undergoing abdominal aortic aneurysm (AAA) repair tend to have higher mortality rates when they are older in age and have comorbidities such as hypertension, peripheral arterial diseases, chronic obstructive pulmonary disease (COPD), and/or chronic kidney disease (CKD). Furthermore, in patients with known CKD, they have also a higher mortality rate within 30-days after operative intervention than those, who do not. This trend is observed with worse severity of CKD, mortality being highest among those patients in CKD stages 3 and 4. It has been suggested that AAA repair should be avoided in patients with CKD unless it is necessary.Our study aimed at validating currently known data using our single-center cohort, and to understand whether these differences are also observed among men and women.
Methods: A single-center retrospective cohort study was conducted between 2002 and 2024. We assessed all adult AAA patients with and without CKD, who underwent open or endovascular aortic aneurysm repair (EVAR or fenestrated-EVAR) at our institution. This project was approved by our institutional review board (IRB 24-004735). Due to the study’s retrospective nature and the subjects’ lower-than-minimal risk, patient consent was waived. After patient identification using
the electronic medical records, those who received an iliac or thoracoabdominal aneurysm repair, and those whose primary AAA repair procedure was performed at an outside institution were excluded from the study. Data extracted from the eligible patients included demographic information, comorbidities, aneurysm details, surgical data, short- and long-term adverse events. The comorbidities for analysis included hypertension, diabetes mellitus, hyperlipidemia, smoking history, CKD and stage, COPD status, coronary artery disease, atrial fibrillation, and stroke following the Society for Vascular Surgery (SVS) practice guidelines. A distinction was made between EVAR and FEVAR because of the increased complications associated with the use of fenestrated grafts.GFR was calculated based on the Modification of Diet in Renal Disease (MDRD) formula. The primary outcome was all-cause mortality on follow-up. Secondary outcomes were 30-day, and long-term complications. Thirty-day complications included in-hospital events that would have delayed the normal postoperative recovery (e.g., hemorrhage, wound complication, mortality), and any other complication from the time of discharge to 30 days after the procedure. Long-term complications included any complication related to the index procedure including wound complications occurring beyond 30-days, hemorrhage, graft thrombosis/infection, and aneurysmal sac growth, among others. A type II endoleak (T2E) immediately post-operatively was not included as a complication. Re-intervention included any additional procedure to treat any endoleak, further aneurysmal degeneration, or complications related to the index surgical intervention for AAA (e.g., embolization, infection). Statistical analysis was performed using R® v.4.4.1. Normal distribution was ascertained by the Shapiro-Wilk test. The categorical variables were analyzed using Pearson’s Chi-squared test, and
continuous variables with non-parametric distribution were analyzed using the Mann-U-Whitney test. A p-value of <0.05 was considered statistically significant. A 1:1 propensity score matched cohort was obtained by a match of age, hypertension, diabetes mellitus, coronary artery diseases, and type of procedure. Survival analysis was conducted between patients with a GFR > 60 mL/min and those with a GFR < 60 mL/min in terms of the primary and secondary outcomes. Log-rank test was used to ascertain differences in the survival analysis. Data was obtained and audited before analysis to reduce information bias. All information was collected sequentially in an encrypted database to ensure patient confidentiality of personal information, reducing the risk of information and selection bias by retrieving the information as needed. This work follows the STROBE criteria.
Results: A total of 292 patients who underwent AAA repair were included. They were categorized into two groups based on GFR: 182 patients had a GFR ≥ 60 ml/min, and 110 had a GFR < 60 mL/min. Before matching, significant differences were observed in hypertension (77.5% vs. 89.1%, p=0.013), diabetes mellitus (12.1% vs. 20.9%, p=0.043), smoking status (p=0.015), chronic kidney disease stages (p<0.001), and coronary artery disease (35.2% vs. 58.2%, p<0.001). Post-matching, these differences were less pronounced without statistical significance between groups in baseline characteristics, for details see
Table I.For the procedural and anatomical variables, the types of procedures performed were similar, with 78.2% vs. 74.5% undergoing EVAR (p=0.74). Aneurysm size was comparable between the groups (mean 53.32 vs. 53.17 mm, p=0.54). Infrarenal aneurysm location was found in 83.6% of patients with GFR ≥ 60 and 79.1% of patients with GFR < 60 (p=0.39). The shape of the aneurysms, presence of rupture at admission, and symptomatic status were not significantly different between groups. The types of grafts used and the specific endograft brands did not show significant differences (all p > 0.05)
(Table II).The length of hospital stay for patients with GFR ≥ 60 and GFR < 60 was similar, with a mean of 2.46 days and 3.2 days, respectively (p=1). The need for intensive care unit (ICU) was not significantly different between the groups (11.8% vs. 17.3%, p=0.25), and the duration of ICU stay also did not show a significant difference (mean 2.5 vs. 4.8 p=0.27)
(Table III).The mean follow-up duration was 2.7 ± 2.9 years for the entire cohort. Long-term complications were similar (19.1% vs. 15.5%, p=0.47), as were 30-day complications (9.1% vs. 11.8%, p=0.51). The presence of T2E at follow-up was not significantly different (33.6% vs. 29.1%, p=0.47), nor was the need for reintervention (19.1% vs. 13.6%), p=0.27). Specific endoleak interventions, including T2E embolization (10.0% vs. 8.2%, p=0.64) and type I endoleak repair (4.5% vs. 2.7%, p=0.47), as well as explants (1.8% in both groups, p=1), were comparable. Notably, all-cause mortality was significantly lower in the GFR ≥ 60 group (13.6% vs. 31.8%, p<0.001) (
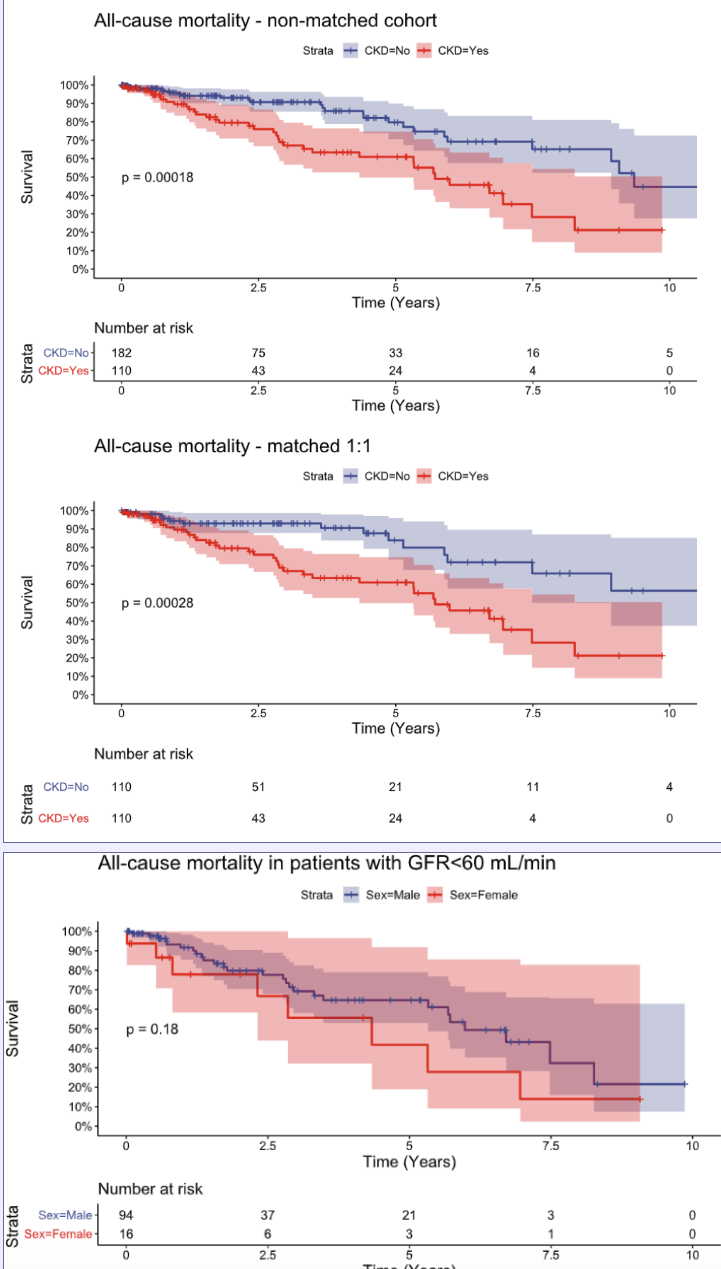
Table III). Survival analysis of all-cause mortality is shown in
Figure 1,
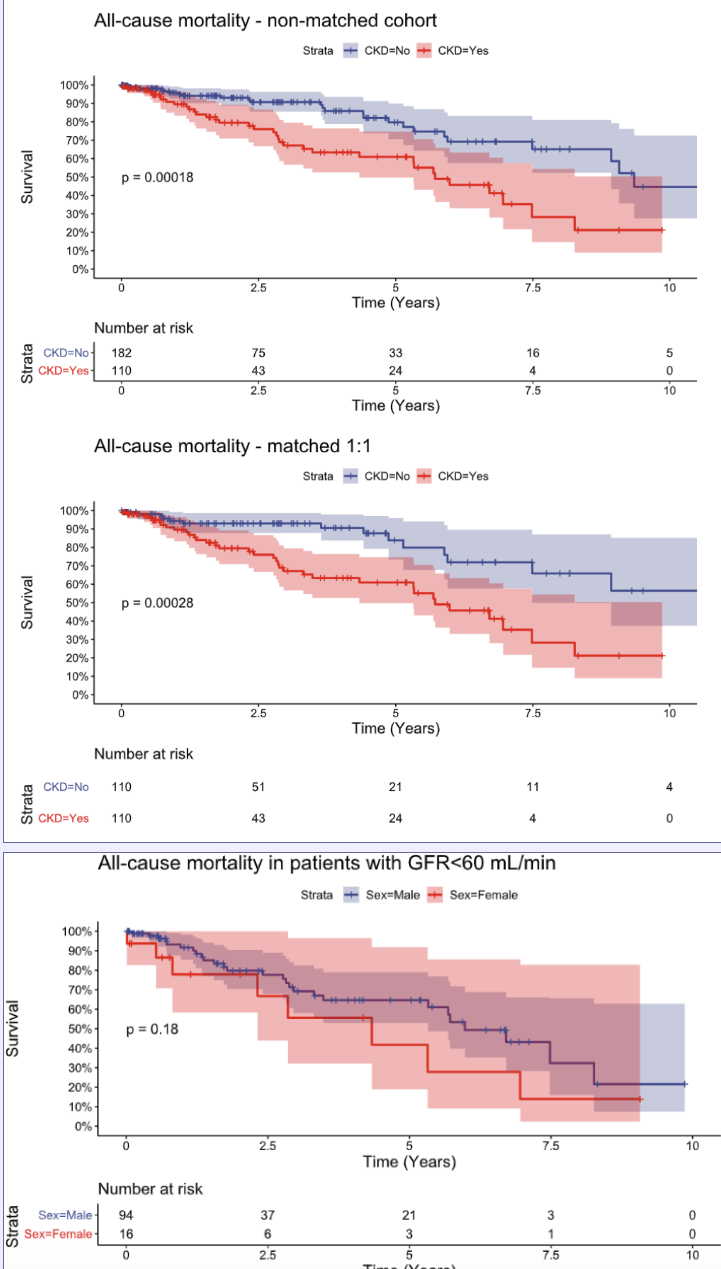
demonstrating statistical significance for all-cause mortality in both matched and non-matched cohorts.We performed an additional analysis to evaluate the differences between sexes with diminished GFR (<60 mL/min) in the whole cohort. All-cause mortality rates were higher in women (50.0%) compared to men (28.7%), though this difference was not statistically significant (p=0.091), please see
Figure 2. There was no significant difference in the rate of 30-day complications between women (18.8%) and men (10.6%) (p=0.35). Long-term complications were less frequent in women (12.5%) compared to men (16.0%) without significance (p=0.72). Re-intervention rates were lower in women (6.2%) than in men (14.9%), but this difference was not statistically significant (p=0.35)
(Table IV).Conclusion: Patients with CKD have a higher all-cause mortality rate on long-term follow-up. Sub-group analysis between men and women demonstrates that sex has no difference in AAA outcomes.
Keywords: Abdominal aortic aneurysm, surgery, chronic kidney disease, cohort study, men vs. women.

Back to 2024 Posters