Back to 2024 Posters
Surgical Reconstruction of the Inferior Vena Cava following Oncologic Resection
Syed Taha Zaidi, Alexander Mills, Ezra Y Koh, Blaz Podgorsek, Ying Huang, Gustavo Oderich, Naveed U Saqib, Sophia Khan
UT houston, Houston, TX
INTRODUCTION: The mainstay of treatment for tumors that involve or encase the inferior vena cava (IVC) is surgical resection with negative margins. The type of reconstruction utilized after resection is dependent on tumor etiology and location. We sought to evaluate our institutional outcomes regarding IVC tumor resection and reconstruction.
METHODS: A retrospective analysis of all patients who underwent IVC reconstruction following en bloc resection at our institution between 2016 to 2022. Medical records were reviewed retrospectively to assess preoperative demographics, perioperative outcomes, and long-term outcomes, including patency, morbidity, and mortality. The primary outcome of interest was the incidence of thromboembolic events following surgery. We analyzed variables across different tumor etiologies, operative approaches, and postoperative antiplatelet therapy or anticoagulation regimens. Additionally, a time-to-event analysis was conducted to compare thromboembolism-free survival days across the various groups, along with an assessment of mortality.
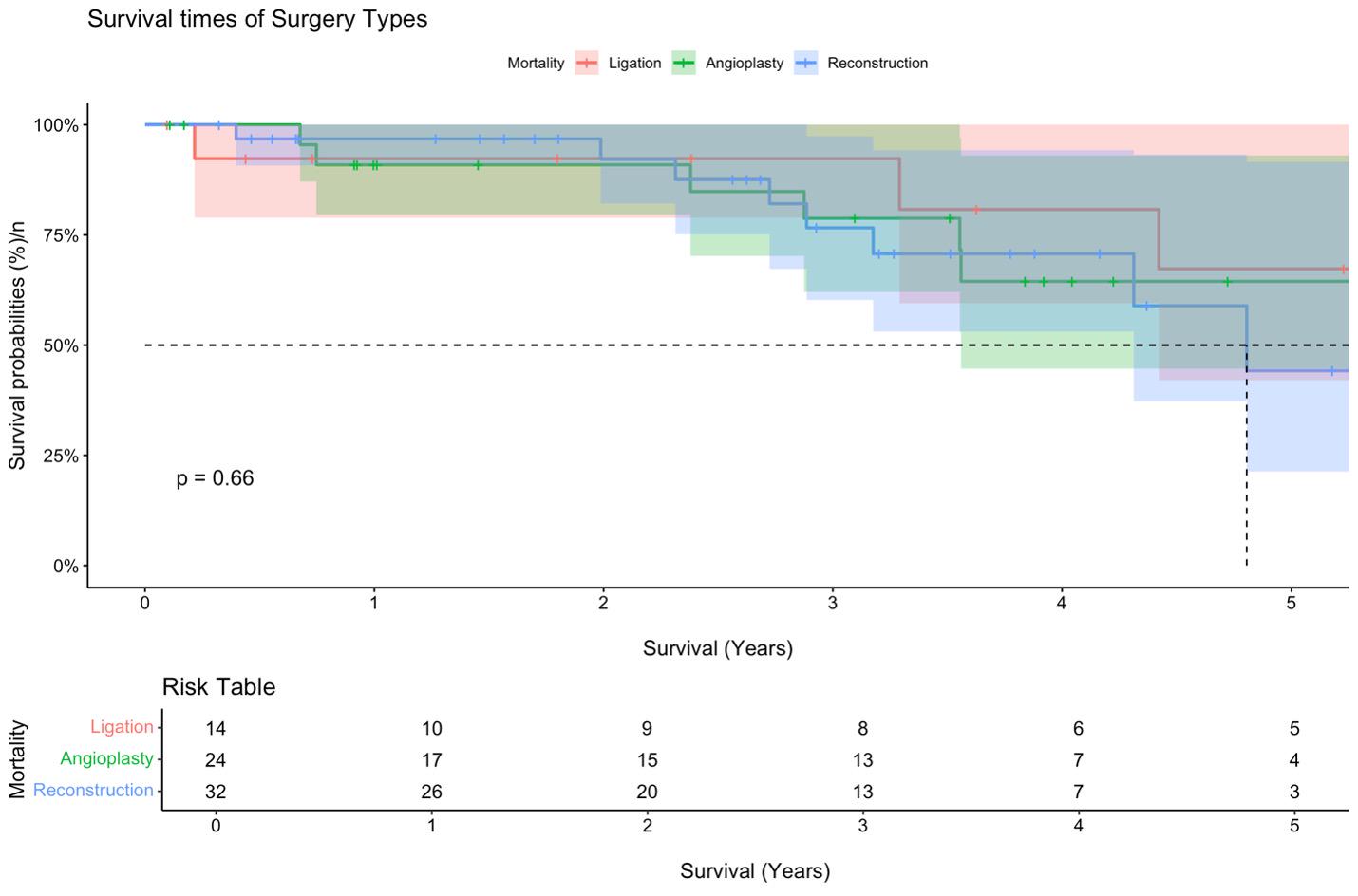
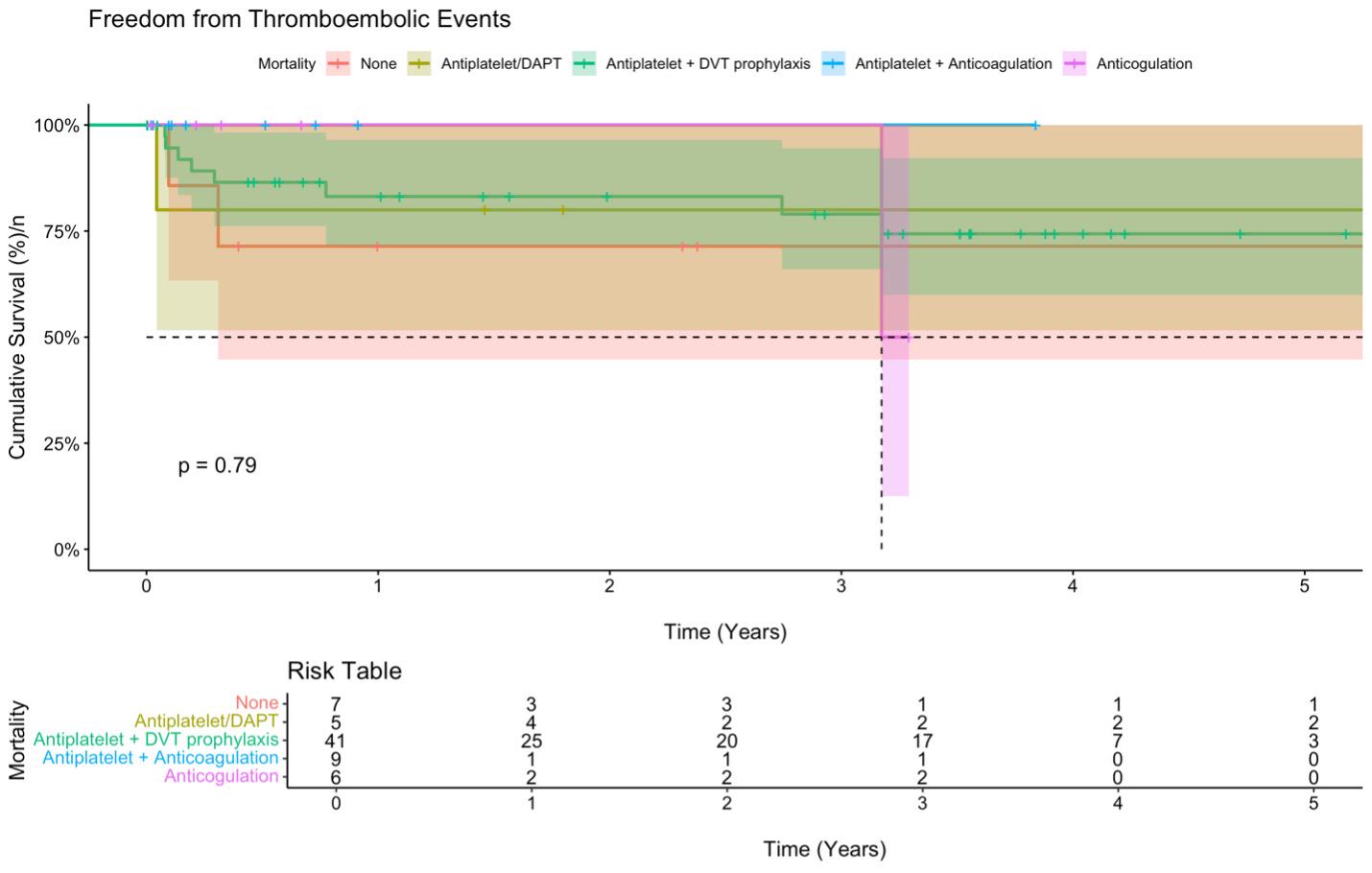
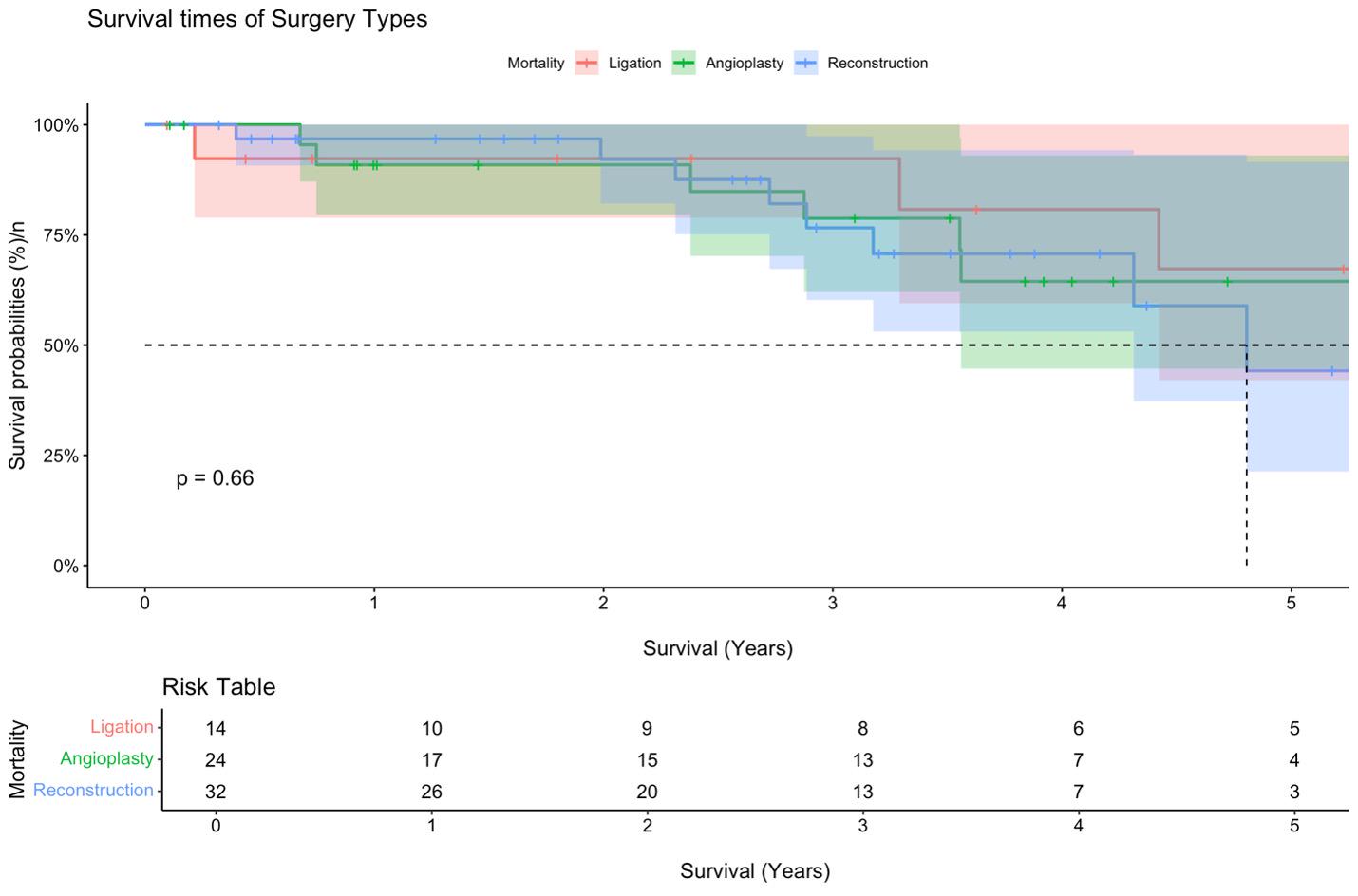
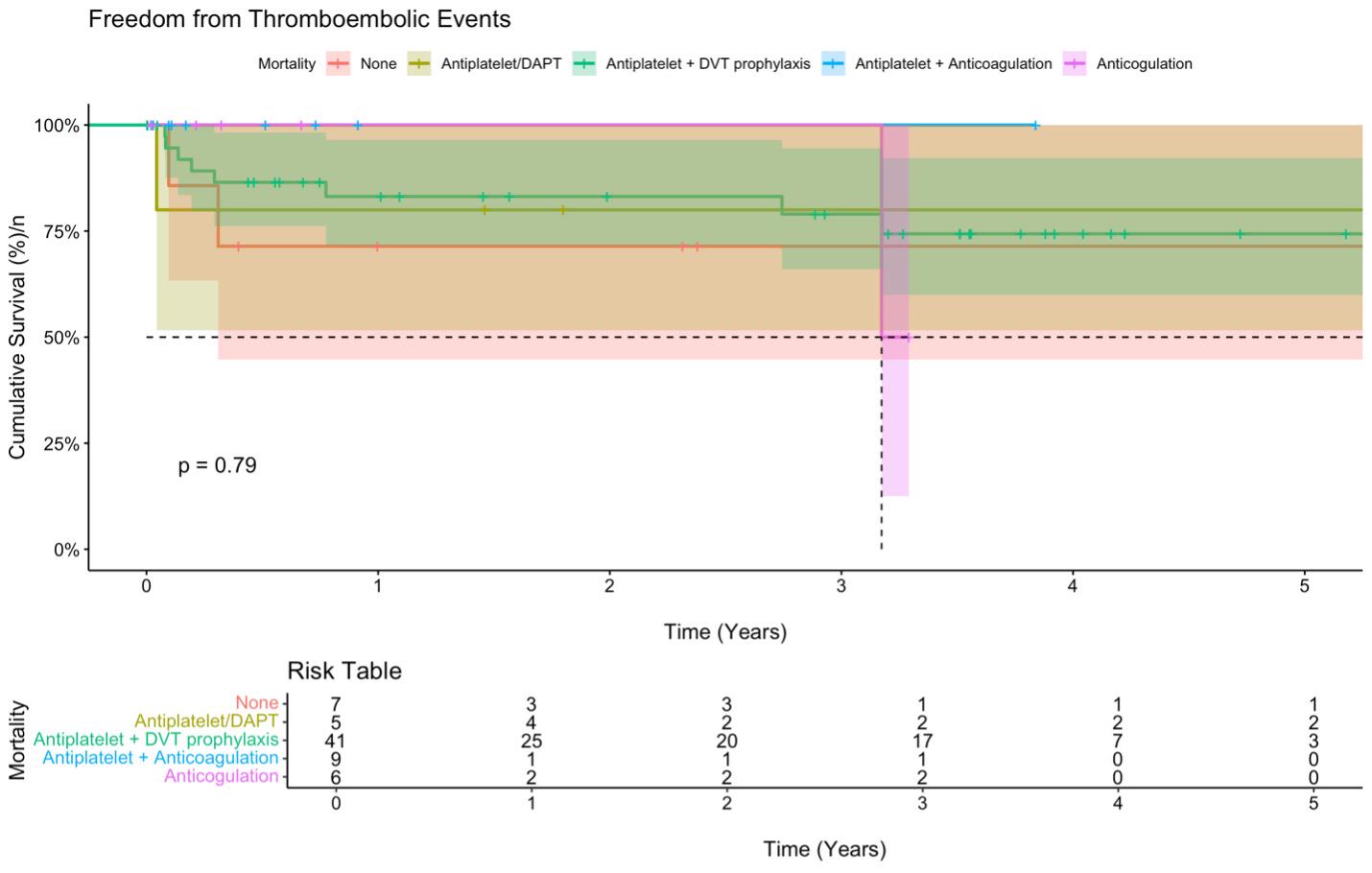
RESULTS: A total of 70 patients underwent IVC reconstruction. Median follow-up was 2.9 years (interquartile range: 1.1 to 4.2). 35 (50.0%) were female, and the median age was 57.0 years (interquartile range: 43.3 to 65.8). The most common diagnosis was leiomyosarcoma (51.4%). Tailored surgical interventions were implemented based on the specific cancer diagnosis, leading to IVC reconstruction with ringed PTFE in 32 out of 70 patients (45.7%), IVC ligation (n=14, 20.0%), or patch angioplasty (n=24, 34.3%). Upon discharge, patients were initiated on varied postoperative regimens, including deep venous thrombosis (DVT) prophylaxis/no therapy (n=7), dual antiplatelet therapy (DAPT) (n=5), antiplatelet with DVT prophylaxis (n=41), antiplatelet with Direct Oral Anticoagulant (DOAC) (n=9), and DOAC alone (n=6). Figure 1 illustrates the survival outcomes among patients undergoing ligation, reconstruction, and patch angioplasty. While survival probabilities decline gradually over time across these surgical approaches, none of the modalities exhibits a distinct survival advantage. The 5-year survival outcomes do not show any statistically significant differences among the three surgical types (p = .66). In contrast, Figure 2 depicts the cumulative survival rate free from thromboembolic events over a 5-year period across various postoperative antiplatelet and anticoagulation therapies. Notably, antiplatelet therapy combined with DVT prophylaxis and antiplatelet plus anticoagulation therapy achieved the highest cumulative survival without thromboembolic events. In contrast, patients who received no therapy experienced a greater incidence of thromboembolic events. Although observable differences exist in thromboembolic event-free survival across these treatment modalities, these differences are not statistically significant (p = .79).
CONCLUSIONS:Our data suggests that survival outcomes are not dependent on surgical reconstruction. Additionally, when compared to the absence of medical therapy, antiplatelet therapy combined with either DVT prophylaxis or anticoagulation showed the highest freedom from thromboembolic events. Although this finding did not reach statistical significance, it suggests that a regimen including antiplatelet therapy and or anticoagulation may offer the most favorable outcomes regarding thromboembolic events.
Back to 2024 Posters