Back to 2024 Posters
The Angle of Anastomosis Should be Considered in Surgical Technique of Lower Extremity Arterial Bypasses
Sarah Allen, Patrick D Conroy, Meghana Mogalipuvvu, Philip M Batista
Cooper University Hospital, Camden, NJ
INTRODUCTION: Lower extremity arterial bypasses are common vascular procedures that can fail for various reasons, including problems with inflow, outflow, conduit, or some combination. Few studies, none-clinical, have demonstrated the effect of the distal anastomosis angle on intimal hyperplasia and bypass failure. In this novel investigation, we hypothesize that the angle of the proximal anastomosis in a lower extremity bypass has a major effect on long-term outcomes and amputation rates.
METHODS: All lower extremity bypasses at our institution were reviewed from 2016-2023. Patients who had lower extremity bypasses with a proximal anastomosis at the common femoral artery were identified, and all patients with postoperative CT scans including the proximal anastomosis were included (n=44). Angles of proximal anastomoses were determined on CT scans using centerline on TeraRecon. Two cohorts, proximal-anastomosis angle < 30° and proximal-anastomosis angle > 30°, were compared. The primary outcome was amputation and graft-occlusion free survival. Secondary outcomes included patency, patency duration, amputation status, and time to amputation. Patency duration was measured from the date of procedure to estimated date of bypass failure, determined by symptom onset with diagnostic evidence of occlusion, amputation date, or explantation. Stata 17.0 was used to perform statistical analysis.
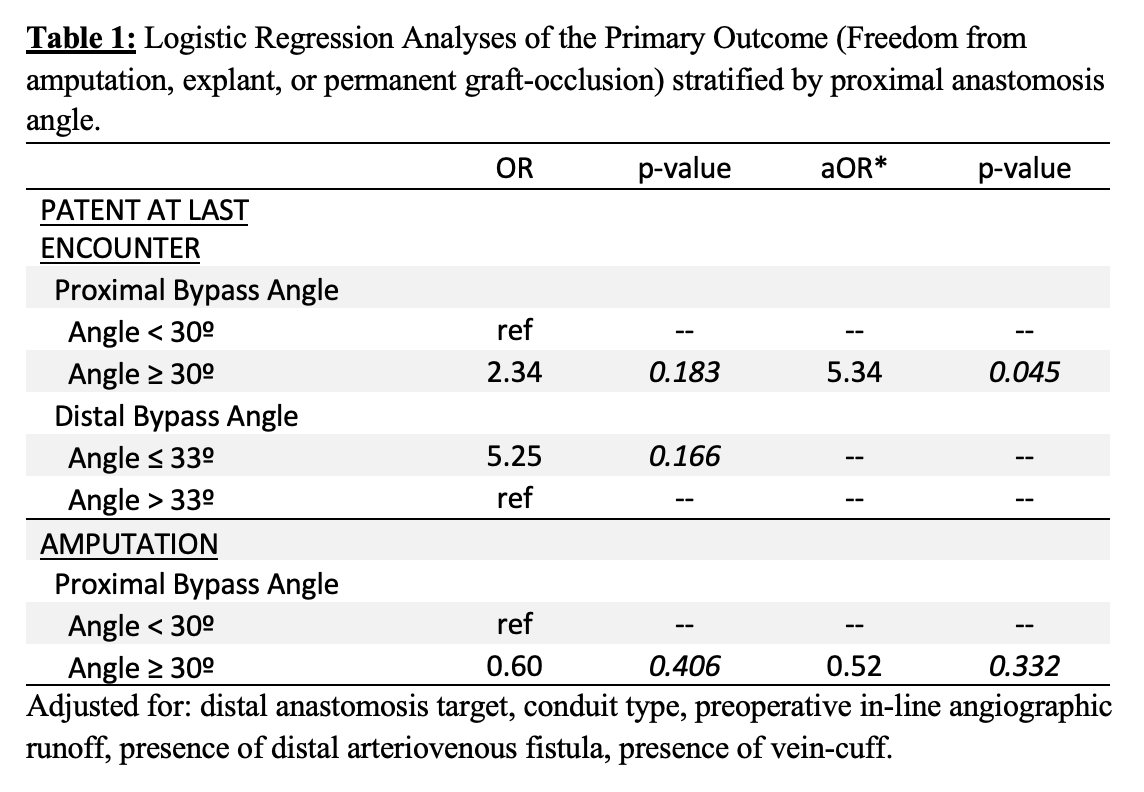
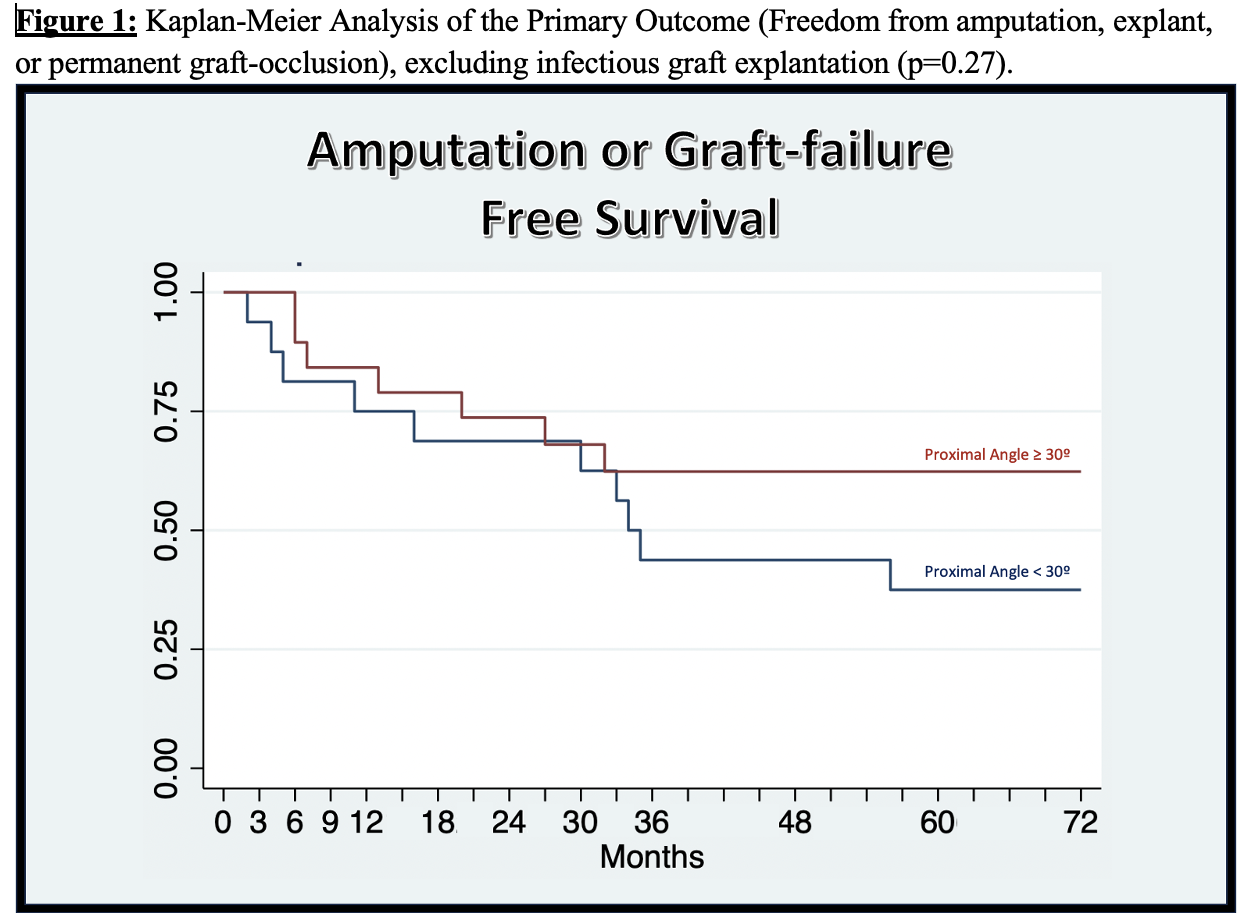
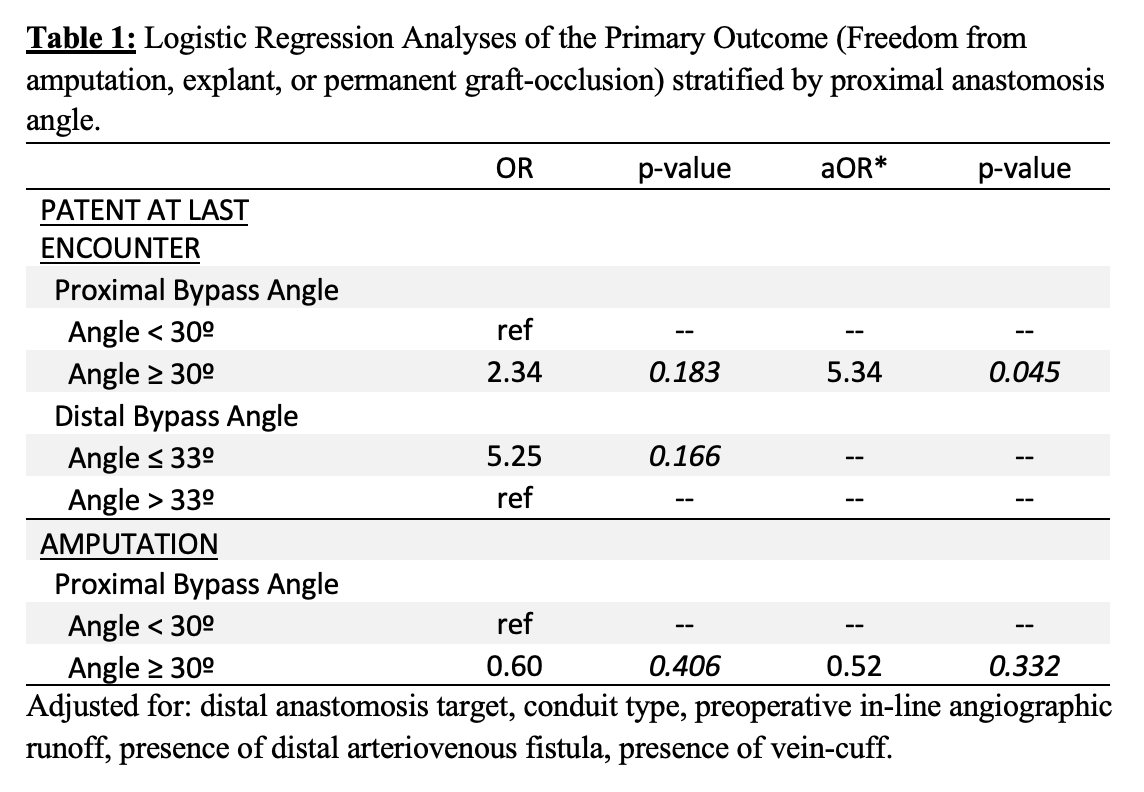
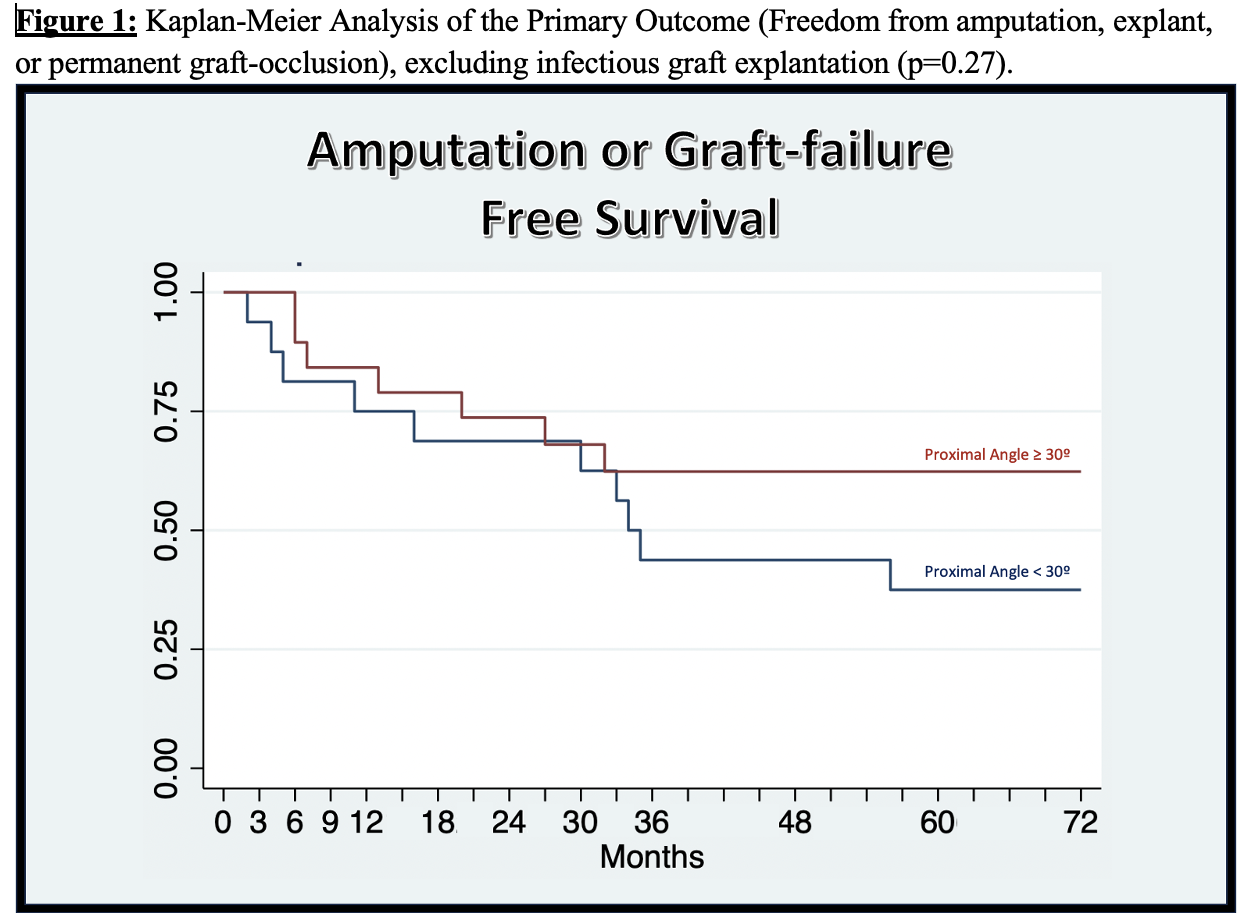
RESULTS: 44 patients were included in this retrospective cohort analysis. The two cohorts were evenly distributed in anatomic and procedural characteristics, most importantly distal anastomosis target, conduit, and in-line target-vessel runoff seen on preoperative angiogram. A proximal anastomosis greater-than-30º was associated with greater rates of freedom from amputation or graft-occlusion (aOR=5.34, p-value=0.045; Table 1), but was not associated with freedom from amputation alone (aOR=0.52, p-value=0.332). A Kaplan-Meier Analysis revealed a nonsignificant trend between a proximal anastomosis angle greater-than-30° and graft survival (no amputation or permanent occlusion; Figure 1).
CONCLUSIONS: We present in our novel analysis that acute-angled (<30º) femoral artery proximal bypass anastomoses are associated with higher rates of graft-occlusion or amputation. This is seen on a high-fidelity regression, adjusted for procedural and anatomic characteristics. Controlling for length of bypass (distal anastomosis site), type of conduit used, and preoperative angiographic in-line runoff, we present compelling results that proximal anastomosis angle is predictive of graft failure and should be considered in future operations. The few nonclinical studies that have investigated anastomosis angles describe more acute anastomosis angles cause more turbulent flow, which they hypothesize to be a causal factor for intimal-hyperplasia. We urge future studies to investigate anastomosis angles in order to potentially guide surgical practice in performing future lower extremity bypasses, to produce bypasses that will lead to longer amputation and graft-failure free survival.
Back to 2024 Posters